What do you see?
CT abdomen and pelvis in the coronal plane
Numbered Findings:
1) Enhancing thickened and narrowed terminal ileum (TI) and cecum. 2)Loculated ascites. 3) Omental cake. 4) Free fluid.
Credit: Ashley Davidoff MD TheCommonVein.net b1511-01b01ES (02Co)
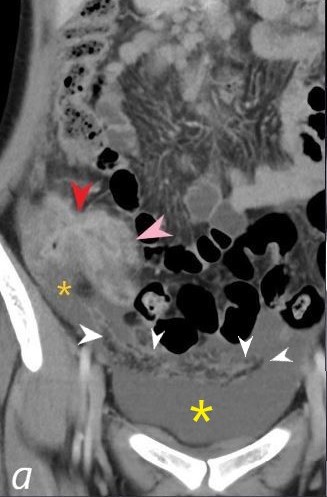
What do you see?
CT abdomen and pelvis in the coronal plane
Numbered Findings:
1) Enhancing thickened and narrowed terminal ileum (pink arrowhead) and cecum (red arrowhead. 2)Loculated ascites (orange asterisk. 3) Free fluid in the pelvis (yellow asterisk) 4) Omental cake (white arrowheads)
Differential Diagnosis : Malignancy (e.g., Adenocarcinoma or Lymphoma) Gastrointestinal Tuberculosis (GI TB): Crohn’s Disease: Yersinia Enterocolitica Infection: Amoebiasis: Actinomycosis:
Comment: Without clinical context, these findings are nonspecific but suggest pathology in the ileocecal region. Clinical correlation is essential to narrow the differential diagnosis. Each of these entities requires targeted workup and management tailored to the clinical setting.
Credit: Ashley Davidoff MD TheCommonVein.net b1511-01bL01ES (02Co)
-
Eye Spy
Title: What do you see?CT abdomen and pelvis in the coronal plane
Numbered Findings:
- Enhancing thickened and narrowed terminal ileum (pink arrowhead) and cecum (red arrowhead.
- Loculated ascites (yellow asterisk.
- Free Fluid (yellow asterisk)
- Omental cake (white arrowheads)
- Differential Diagnosis:
- Malignancy (e.g., Adenocarcinoma, Lymphoma, or Appendiceal Tumors):
- Cecal or ileal tumors can cause bowel thickening and luminal narrowing.
- Appendiceal tumors (e.g., mucinous neoplasms, adenocarcinomas) can cause omental caking and ascites, mimicking peritoneal carcinomatosis.
- Lymphoma: May occasionally cause omental caking, often with lymphadenopathy or bulky mesenteric masses.
- Clinical context: Older patients, systemic symptoms like weight loss, and absence of granulomatous inflammation.
- Gastrointestinal Tuberculosis (GI TB):
- Commonly involves the terminal ileum and cecum.
- Associated with granulomatous inflammation, focal bowel thickening, ascites, and omental caking.
- Mycobacterium bovis: More frequently linked to ingestion of unpasteurized dairy products (prevalent in Africa, South Asia, and Latin America).
- Mycobacterium tuberculosis: Can cause ileocolic disease via hematogenous or lymphatic spread, particularly in active pulmonary or miliary TB.
- Crohn’s Disease:
- Chronic inflammatory bowel disease with characteristic skip lesions.
- Thickened bowel walls and narrowing may overlap with other conditions.
- Ascites and omental caking are uncommon.
- Key point: Omental caking is not usually seen in Crohn’s disease, and its presence would effectively exclude this diagnosis.
- Clinical context: Younger patients, perianal disease, and extraintestinal symptoms (e.g., arthritis).
- Yersinia Enterocolitica Infection:
- Mimics TB in the ileocecal region with wall thickening and mesenteric lymphadenopathy.
- Ascites is less common, and omental caking is rarely seen.
- Key point: Omental caking’s presence would exclude this diagnosis.
- Clinical context: Febrile illness and gastrointestinal symptoms after ingestion of contaminated food.
- Amoebiasis:
- Caused by Entamoeba histolytica.
- Leads to colonic thickening and possibly cecal involvement.
- Ascites is less typical, and omental caking is not a common feature.
- Key point: Omental caking’s presence would effectively exclude amoebiasis.
- Clinical context: History of travel to endemic areas.
- Actinomycosis:
- Rare bacterial infection presenting as mass-like bowel thickening, often mimicking malignancy or TB.
- Fistulas and abscesses are common.
- Omental caking is very rare in actinomycosis.
- Key point: Omental caking’s presence would exclude this diagnosis.
- Clinical context: Dental infections or GI trauma as potential predisposing factors.
Comment:
- Omental caking is a key radiologic finding often associated with gastrointestinal tuberculosis, malignancy (particularly appendiceal neoplasms or peritoneal carcinomatosis), and occasionally lymphoma.
- Its presence significantly narrows the differential diagnosis by excluding conditions like Crohn’s disease, Yersinia enterocolitica infection, and amoebiasis, which rarely cause omental caking.
- Clinical correlation is essential to determine the underlying etiology.
- Each of these entities requires targeted workup and management tailored to the clinical setting.
Credit: Ashley Davidoff MD TheCommonVein.net b1511-00a (02Co)
- Malignancy (e.g., Adenocarcinoma, Lymphoma, or Appendiceal Tumors):
Links and References
1.ACG Clinical Guideline: Management of Crohn’s Disease in Adults. Lichtenstein GR, Loftus EV, Isaacs KL, et al. The American Journal of Gastroenterology. 2018;113(4):481-517. doi:10.1038/ajg.2018.27.
3.Lymphoma: Diagnosis and Treatment. Lewis WD, Lilly S, Jones KL. American Family Physician. 2020;101(1):34-41.
Turlakow A, Yeung HW, Salmon AS, Macapinlac HA, Larson SM. Journal of Nuclear Medicine : Official Publication, Society of Nuclear Medicine. 2003;44(9):1407-12.
5.Yersiniosis. Louise Francois Watkins, Cindy Friedman CDC Yellow Book
6. Assessment of Adult Women With Ovarian Masses and Treatment of Epithelial Ovarian Cancer: ASCO Resource-Stratified Guideline. Vanderpuye VD, Clemenceau JRV, Temin S, et al. JCO Global Oncology. 2021;7:1032-1066.
7. Retrospective Case-Control Study to Predict a Potential Underlying Appendiceal Tumor in an Acute Appendicitis Context Based on a CT-scoring System. Monsonis B, Zins M, Orliac C, et al. European Journal of Radiology. 2021;136:109525. doi:10.1016/j.ejrad.2021.109525.