Virtual Colonography
Copyright 2008
Definition
CT colonography is a computer generated image of the colon that simulates colonoscopy. It is used for patients who require screening examination for polyps and cancer. Optical colonoscopy is the study of choice in these patients because if there are findings then the patient can be biopsided. However about 10% of these patients optical colonoscopy fails and CT colonoscopy offers an alternative, safe and sccurate test.
indicated in allpatients over 50 years but the study requires expert gastroenterologists, requires concious sedation
CT colonography (CTC) or virtual colonoscopy is an examination in which advanced reconstruction techniques are applied to data obtained from abdominal CT, to generate images of the colon.
CT Colonography
(Virtual Colonoscopy)
The Common Vein Copyright 2008
Scott Tsai MD Ashley Davidoff MD
Definition
CT colonography (CTC) is a diagnostic imaging tool that consists of computer generated images of the colon acquired through high resolution CT. The procedure simulates colonoscopy, and is therefore also known as virtual colonoscopy. It is highly sensitive to surface evaluation of the mucosa of the colon, and is able to detect lesions as small as 5mm. It is therefore used to aid in the diagnosis of colonic polyps and colonic carcinoma. It is performed as an outpatietnt procedure, requires bowel cleansing and distension of the colon with air and otherwise has little risk to the patient. Its main current indication is for patients who have had a failed colonoscopy, but it is being considered as an alternate method to colonoscopy for screening for polyps and cancer since this is recommended for all patients over 50 years.
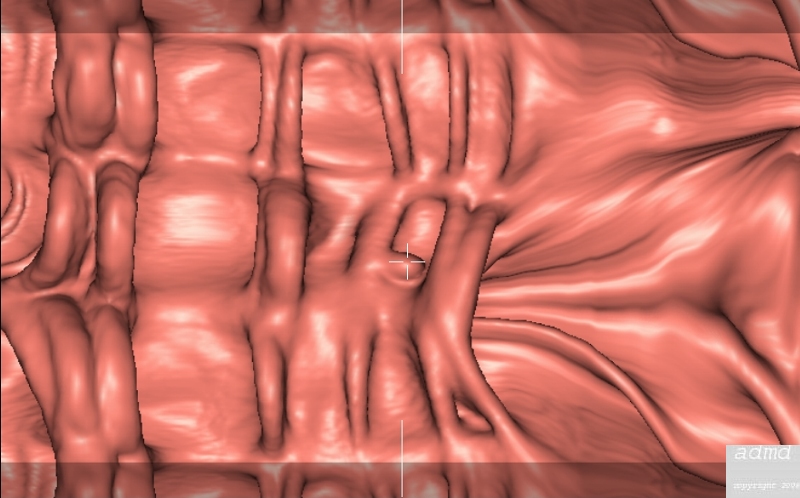
Fly through View Normal Left and Carcinoma Right |
| 75420b03 fly through view colon cecal carcinoma mass CT colonography virtual colonoscopy CTscan Courrtesy Scott Tsai MD |
|
Principles Copyright 2008 Introduction The purpose of the module is to provide an understanding of how best to achieve a useful and effective diagnostic study of the colon for the purpose of identifying small and potentially malignant disease. This project therefore requires an understanding of the structure and function of the colon , the diseases that we are looking for, and an understanding of the imaging technology we are using.
As a summary to the evolving module it is reasonable to introduce the subject by providing a big picture of these principles.
The colon is a capacious muscular tube that is designed for mixing and churning, water reabsorbtion, and massive peristaltic movements to evacuate solid material. It is a distensible structure that is characterized on its inner surface by mucosal folds. In our attempts to identify the abnormal mucosa it is imperitive that we distend the colon so that we reduce the accordion effect of redundant mucosa. By distending the colon we open all the surfaces so that small space occupying abnormalities are not hidden. Since the colon usually contains stool and debris it is imperitive that the surface does not contain flecks of debris that may be misconstrued. as disease. The two basic diseases we are looking for include polyps and cancer and both arise from the mucosa.
Imaging structure requires that two structures that lie side by side are sufficiently different in character that they can be identified. The introduction of air into the colon allows a distinction to be made between the lumen and the surface of the mucosa. Imaging is best performed when we can freeze time in a moment, so that if exposure time is reduced then we avoid motion artifact. The MDCT technology has enabled us to shorten exposure times and hence obtain clearer pictures. The technology has also enabled improved spatial resolution and the acquisition of volumetric data. Volumetric CT data of the entire colon are acquired and combined with advanced imaging software to allow analysis at a dedicated workstation so that 2D and 3D images can be reviewed (2). |
Principles of Imaging
The Common Vein Copyright 2008
Principles in Imaging
CT colonography is a high resolution isovoxel imaging technique where the surface of the colon is the target of the technique. The contrast difference between the surface of the colon and the lumen is created by infusion of air into the lumen creating an exquisite density difference between the soft tissue density of the mucosa (20-40HU) and that of the air (-1500 HU) is created.
Data is obtained from helical CT scanning and commercially available software, allows postprocessing of data:
Two techniques are used; surface rendering and volume rendering. Surface rendering links the contours of selected objects. It is faster in processing but subject to poor definition, data loss, and threshold artifacts.1 Volume rendering allows for more detail and opacity but entails increased processing time and cost.
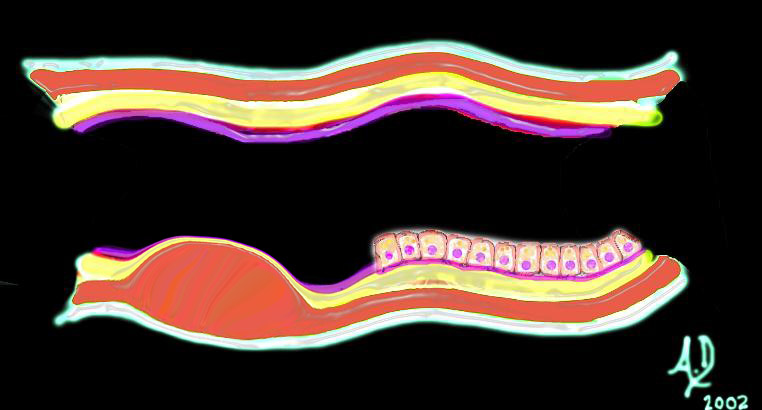
The polyp is seen as a nodule on the surface of the bowel and because it arises from the mucosa the angles created with the mucosa are acute.
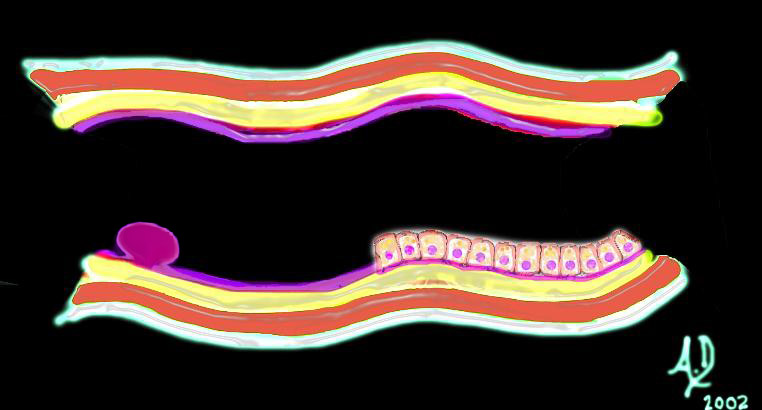 Mucosal Lesion Acute Angles with the Surface Mucosa Mucosal Lesion Acute Angles with the Surface Mucosa |
| 32347d01 mucosa submucosa muscularis adventitia serosa mucosal mass polyp neoplasm carcinoma acute angles with the lumen histopathology imaging diagnosis Davidoff art Davidoff MD |
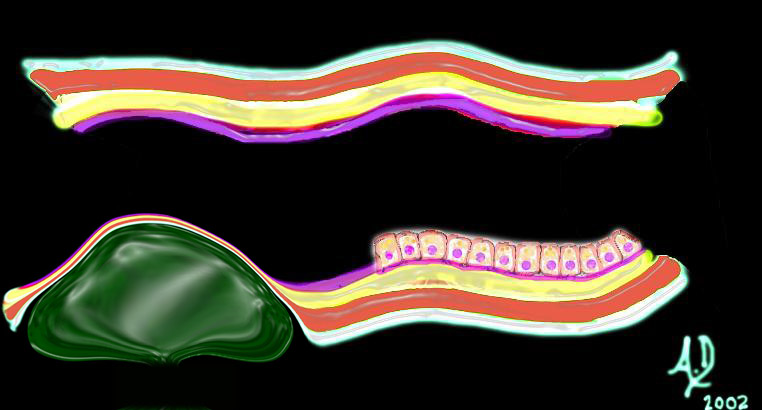
Diseases that affect the submucosa such as edema, or hemorrhage, or inflammation cause a heaping up of the mucosa, and the shape of a submucosal lesion is quite different. It is seen by the endoscopist, or double contrast enema as a heaped up lesion with obtuse angles. Lesions of the submucosa may occur in acute inflammatory or ischemic diseases, or in neoplastic diseases such as lymphoma or lipomas. Lesions arising from the muscularis, such as leiomyomas also create an obtuse angle (and sometimes a right angle with the mucosal surface.
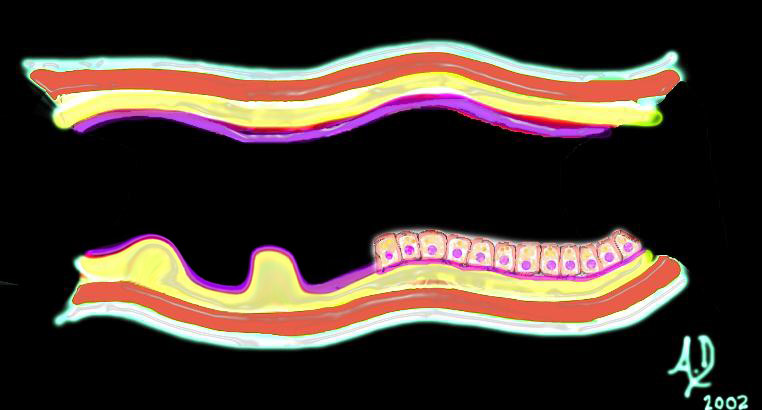 Submucosal Lesion Obtuse Angle or Right Angle Submucosal Lesion Obtuse Angle or Right Angle |
| 32347d02 mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage obtuse angles or right angle 90 degree ninety degree angle with the lumen histopathology imaging diagnosis Davidoff art Davidoff MD |
 Lesion Arising From the Muscularis – Obtuse Angles Lesion Arising From the Muscularis – Obtuse Angles |
| 32347d03 mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage obtuse angles or right with the lumen histopathology imaging diagnosis Davidoff art Davidoff MD |
| Extrinsic |
| 32347d04 mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage neoplasm malignancy benign obtuse angles with the lumen histopathology imaging diagnosis Davidoff art Davidoff MD |
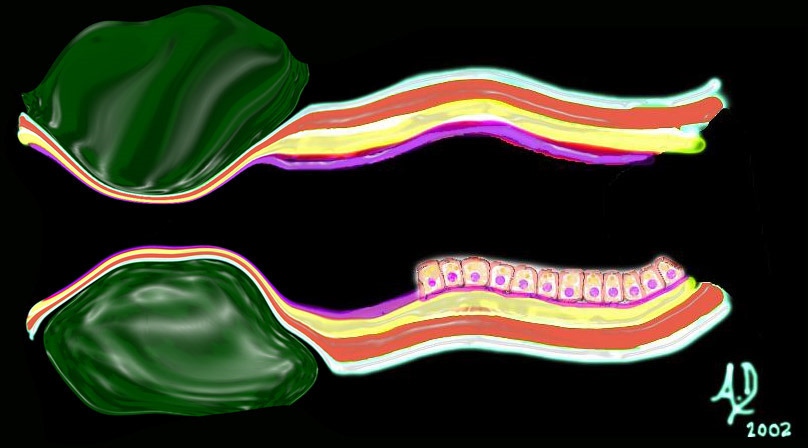
Extrinsic |
| 32347d06 mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage neoplasm malignancy benign obtuse angles with the lumen histopathology imaging diagnosis Davidoff art Davidoff MD |
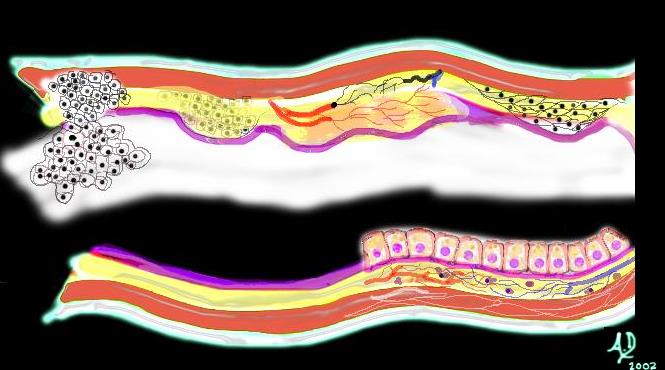 Malignant and aggressive growth Malignant and aggressive growth |
| The diagram illustrates the transformation from benign to malignant as the neoplasm starts to reveal an aggressive nature and invades and destroys surrounding tissue. In this instance it has advanced into the submucosa and muscularis as well as expanded into the lumen.
Courtesy Ashley Davidoff MD |
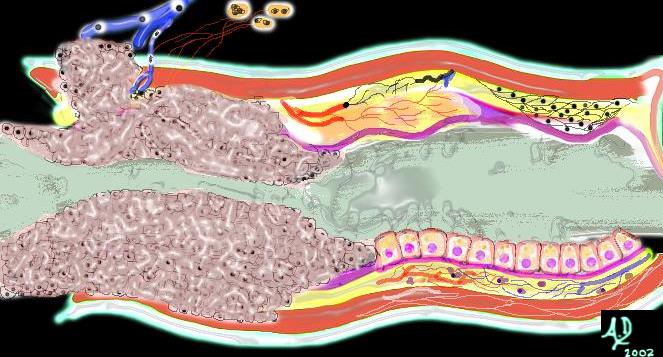 Malignant growth through the all into veins and nodes Malignant growth through the all into veins and nodes |
| Left undiagnosed and untreated the malignant cells continue to grow without regard to the neighboring structures. It encircles the colon in “napkin-ring” fashion (as shown above) eventually blocking off the lumen and causing a bowel obstruction. It may grow through the wall and cause a bowel perforation and or grow into regional lymph nodes and portal venous radicles after which it will metastasize to the liver and other organs.
Courtesy Ashley Davidoff MD 32367b01 |

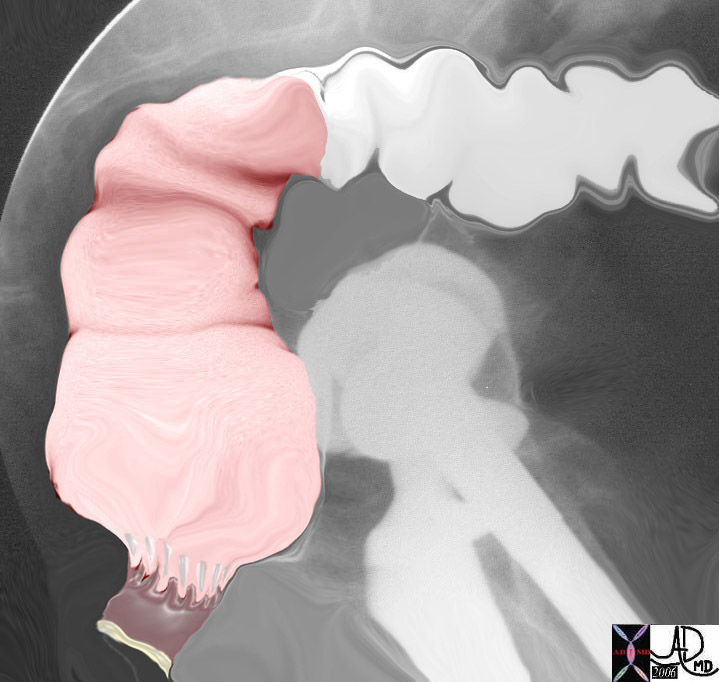
5mm benign polyp |
| This 5mm polyp is a common finding on colonic evaluation and at this size is a benign abnormality. Left intact it can grow into a monster. Hence it is usually removed by the endoscopist.
Courtesy Ashley Davidoff MD 12087 |
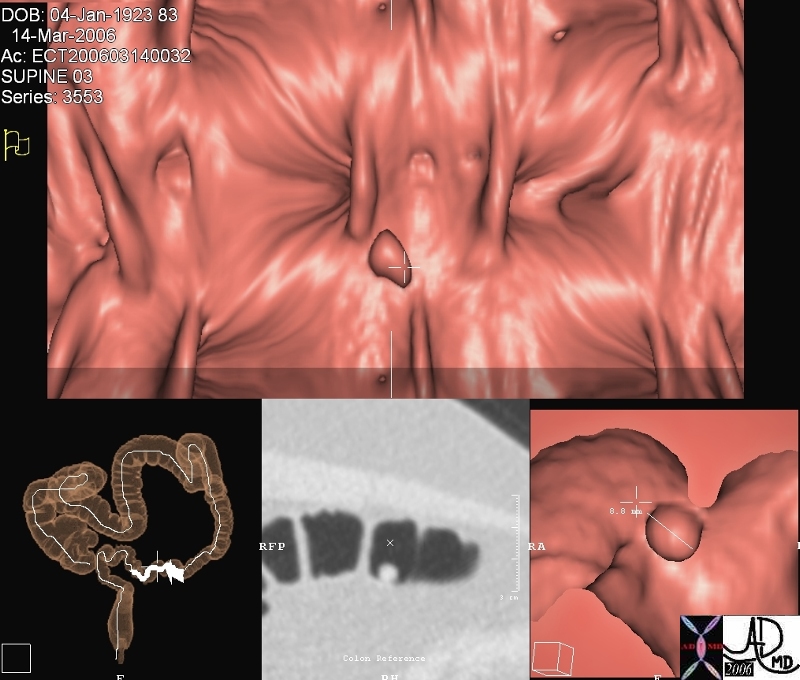
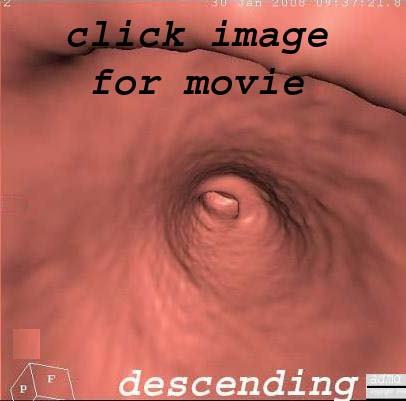
This series of images from a virtual colonoscopy shows an 8 mms polyp seen on the surface rendering images (salmon colored images) referenced to the sigmoid colon (bottom left) and with conventional CTimaging (bottom middle) At this size the polyp is almost certainly benign and can be removed through the colonoscope safely. Note in the gray scale image (middle image 2nd row) the acute angles formed by the polyp with the underlying mucosa. The distal location raises the likelihood that it represents a hyperplastic polyp.
Courtesy Scott Tsai MD
45119
|
Indications Copyright 2008 Indications for CT colonography include;
The examination is a promising test likely soon to be used routinely for colorectal cancer screening. Many studies indicate the efficacy of CTC. Preliminary results of a multicenter national trial of 2,531 patients reveals that CTC (VC) is as sensitive to 1cms polyps as optical colonoscopy. The study was conducted by the American College of Radiology Imaging Network, and funded by NIH . The results are expected to promote CTC into the frontlines of colorectal cancer screening. |
Advantages
The gold standard for polyp and cancer detection is optical coloscopy since it is both a diagnostic and potentially therapeutic procedure..
The advantages of CT colonography include;
– absence of a need for sedation
– lower risk for perforation
– less expensive
– ability to detect extra-colonic findings
In up to 40% of patients undergoing CTC extracolonic abnormalities are detected. 14% of these incidental findings require further investigation, and the incidence of finding significant disease was 1in 200. eg aortic aneurysms and extra-colonic malignancy. (Xiong)
Disadvantages
Radiation
The procedure does involve radiation, but the risks of developing colon cancer are far higher than the risks of developing cancer from the radiation. The radiation dose is about 5 mSv for men, 7.8 mSv for women (2)
The radiation dose is an issue especially for a screening test. Attempts have been made too reduce the radiation, by taking advantage of the fact that there is high contrast between a polyp projecting into the lumen of an air distended colon to lower the radiation dose to a patient. Because of this inherent high contrast, the mAs, (X-ray parameter that is the product of the x-ray tube current and exposure time,) can be decreased, and still the polyp can be visualized. mAs is proportional to absorbed dose, so decrease in mAs leads to decrease in dose. A typical mAs for routine abdominal CT for example is 200 but for VC it can be decreased to 50.
By doing this, the dose to a patient for VC is comparable to a barium enema and it is less than a routine abdominal CT.
Imaging Test Effective Dose Equivalent (mSv)
Chest X-ray 0.01 – 0.05
Abdominal X-ray 0.6 – 1.7
Barium exam 3 – 8
Head CT 2 – 4
Chest CT 5
Abdomen CT 10
Virtual colonoscopy 5 – 7.8
Cardiac CT (64-slice) 10 – 15
Selective coronary angiography 5
Yearly natural background 3.6
Need for Further Intervention
A second disadvntage is is the need for a colonoscopy if the study is positive. If a polyp or cancer is found the patient by CT clonography, the patient will still require an additional colonoscopy to obtain a biopsy and or have the polyp endoscopically removed.
Discomfort of the Preparation
The study does require a cleansing preparation which is an uncomfortable 48 hour preparation of liquid diet and 24 hour period of induced diarrhea.
References
Xiong T et al. Incidental lesions found on CT colonography: their nature and frequency. British Journal of Radiology (2005) 78, 22-29.
Contraindications
– patients who are unable to perform bowel cleansing or colonic distension
Patient Preparation
The Common Vein Copyright 2008
A good bowel preparation is crucial for successful performance of the examination since residual fecal material is the most common cause of false positives. Dietary restriction and laxatives are the main components of bowel prep. Patients are restricted to a clear liquid diet 24 hours prior to the examination. A two dose regimen of 45 mL of phospho soda is the preferred agent since it leaves the colon drier than polyethylene glycol, so that residual fluid in the colon does not hide polyps. However, phospho soda should be avoided in patients with renal, cardiac or hepatic insufficiency.
Compliance for colorectal cancer screening would likely increase if CTC could be performed with minimal or no bowel preparation. Low compliance for screening has been linked to pervceived discomfort of the examination technique and pre-exam preparation. Fecal tagging refers to administration of oral agents that would mark fecal material in the colon so that these could be distinguished from polyps. Furthermore, electronic cleansing refers to application of image processing techniques to remove marked contents from the CTC images themselves.Fecal tagging, although not a mandatory requirement of the examination, can help in differentiating residual stool from polyps. A suspension of barium sulphate is ingested with the clear liquid diet. Any residual stool becomes coated with the barium and can be differentiated from polyps.
Preparing the Colon
Patient preparation prior to the exam is a critical step, and perhaps the most important part of the test. Just as with conventional colonoscopy, a fully prepared colon is necessary.
Aim
A clean dry and distended colon are the three factors that are needed to obtain a good quality study.
Method
Phospho soda
Phospho soda, a cathartic, is the preferred method, leaving the colon clean and dry but cannot be used in patients with
cardiac, renal or hepatic insufficiency.
The phospho-soda preparation kit contains 45 mL of monobasic sodium phosphate, four bisacodyl laxative tablets, and one bisacodyl suppository
Clear Liquid Diet reference
The preparation may result in acute elevation of serum sodium concentration, it is contraindicated in patients with congestive heart failure or renal failure.
The sodium phosphate that the patient takes orally acts as an osmotic cathartic and the bisacodyl as a colonic stimulant. This combination, as well as the decreased total volume that needs to be ingested with this preparation, may account for the decreased colonic fluid noted with use of the phospho-soda preparation in our study.
Go Lytely (polyethylene glycol) is a GI lavage can be used in patients who should not take phospho soda, but there is the potential for large amounts of residual fluid.
Patient drinks clear liquids for twenty four hours before the test.
Stool tagging is performed by drinking three 20 mL bottles of dilute barium so that it can mix with any retained stool, making it distinguishable from polyps and reducing false positives.
| Small Amount of Fluid In the Colon is Acceptable |
| 75372c01 colon cecum air fluid level supoptimal prep poor preparation CTscan CT conography Virtual Colonoscopy Courtesy Ashley Davidoff MD |
Preparing the patient
Allay fears and provide information
The patient is usually nervous about the procedure, sometimes related to privacy issues, and sometimes related to the invasive nature and potential discomfort.
Method
A quiet empathetic and confident approach is necessary.
Inform the patient that the exam takes about 10 minutes and that no sedation is necessary.
The patient should be told that the catheter is relatively small, that it will be lubricated and inserted slowly and gently while they lie toward the wall with hips and knees flexed. If there is discomfort slow in and out breathing will help.
They should also be informed that a small balloon will be inflated once the catheter is inserted which will create a full feeling in the rectum. Once this is done they will be asked to puff the catheter to fill the colon with air. The distension is a critical part of the exam and the patient should try to hold the gas as much as possible. Either room air or carbon dioxide can be used. Room air is easier to use, provides longer retention time and does not require additional equipment to use. Patients however find carbon dioxide easier to tolerate as it is easily absorbed after the exam, thereby reducing abdominal cramping. Most institutions use room air.
The first part of the test they will lie supine and the second part they will lie prone in order to move the air around and optimally evaluate the full circumference of the colonic wall.
After the exam the study requires processing and the radiologist will reconstruct the colon and evaluate the images.
The patient should be told that they may still need a colonoscopy if a polyp is found in order to obtain a biopsy.
After the exam they will find that they will pass excessive amounts of gas. They should not have any other symptoms but if they have prolonged pain after the procedure they should call their doctor.
Complications
Information about complications is necessary. The risk of perforation is extremely low.
Equipment
Tubes and Pump
The tubing can be either a small rubber tube, but a balloon tipped catheter is often used since it is more stable and less likely to come out.
A hand held bulb syringeis an einexpensive mechanism to insufflate room air. A automatic insufflator for carbon dioxide is a more expensive and slightly more comfortable alternative technique.
Multidetector CT scanner
With current state of the art muti-detector CT scanners, large data volumes can be obtained in short acquisition times decreasing respiratory motion artifact. For example, single detector scanners acquiring 5 mm thick sections and pitch of 2, typically require 35 to 40 seconds to scan the abdomen and pelvis. This yields effection section thickness of 6.4 mm. In contrast, 16 dectector CT scanners can scan the same z-axis coverage in 15 to 20 seconds with 0.75 mm collimation and a pitch of 1.5 with data reconstructed at 1 mm overlapping every 0.75 mm. A 64 detector row scanner acquires similar data in less than 10 seconds. The ability to acquire thin section overlapping images optimizes 3D reconstructions. Near isotropic voxels can be obtained which allow for multiplanar reformations and endoluminal images which are important in distinguishing polyps from bulbous folds and residual fecal material.
Software
The need to frequently distinguish between polyps and flecks of stool requires the use of evaluating the finding using both 2D and 3D techniques. This requires the use of a dedicated workstation and CT colonography software for image processing.
Technique
The Common Vein Copyright 2008
Introduction
Many parameters are important for successful performance of CTC. Factors include bowel cleansing, fecal tagging, colon insufflation as described above.
CT colonography (CTC) requires MDCT technology, trained technologists and radiologists, and advanced reconstruction techniques. Computer aided detection and minimal prep CTC are advances that can improve the accuracy and compliance of the exam.
With current state of the art muti-detector CT scanners, large data volumes can be obtained in short acquisition times decreasing respiratory motion artifact. For example, single detector scanners acquiring 5 mm thick sections and pitch of 2, typically require 35 to 40 seconds to scan the abdomen and pelvis. This yields effection section thickness of 6.4 mm. In contrast, 16 dectector CT scanners can scan the same z-axis coverage in 15 to 20 seconds with 0.75 mm collimation and a pitch of 1.5 with data reconstructed at 1 mm overlapping every 0.75 mm. A 64 detector row scanner acquires similar data in less than 10 seconds. The ability to acquire thin section overlapping images optimizes 3D reconstructions. Near isotropic voxels can be obtained which allow for multiplanar reformations and endoluminal images which are important in distinguishing polyps from bulbous folds and residual fecal material.
Computer aided detection (CAD) is a technology routinely used in mammography. Computer aided polyp detection for CTC is currently being developed. A high sensitivity and low false positivity algorithm is desired. Clinical trials are underway to assess the application of CAD to clinical practice.
Tube Insertion
The patient is positioned facing away from the attendant and asked to flex knees and hips. Prior to inserting the tube the patient is told to slowly breathe in and out through the mouth if there is discomfort.
The small tube or barium tip is lubricated, the upper buttock cheek is pushed upward exposing the anus. The tip is slowly inserted pointing the tip in the direction of the patients umbilicus. Initial resistance of the anal sphincter will be followed by a “give” of the resistance as the the anal sphincter is traversed, and the tip is advanced by about two more inches.
 Anus is directed anteriorly and Upward Anus is directed anteriorly and Upward |
| 29814b013 colon rectum large bowel sigmoid colon rectosigmoid anus anal canal pectinate line rectal columns rectal sinuses anorectal junction anatomy lateral examination sacrum barium enema BE imaging radiology contrast X-Ray Davidoff art Courtesy Ashley Davidoff MD |
The patient is returned to the prone position and given the hand pump for self insufflation
Colonic Distension
Either room air or carbon dioxide is utilized. Colonic distension is achieved in our institution with room air can be administered manually with a hand held bulb syringe by asking the patient to pump 40-50 times and once reached – asked to pump about 10 more times until he/she feels some discomfort. Alternatively, mechanical insufflation devices can be used that administer carbon dioxide to a set pressure and maintains the pressure throughout the exam. Both room air and carbon dioxide are equally effective, however, CO2 is more readily absorbed from the colon and therefore is more comfortable because there is less cramping after the test.
Scout Film
A scout scan in the supine position verifies that adequate distension has been accomplished.
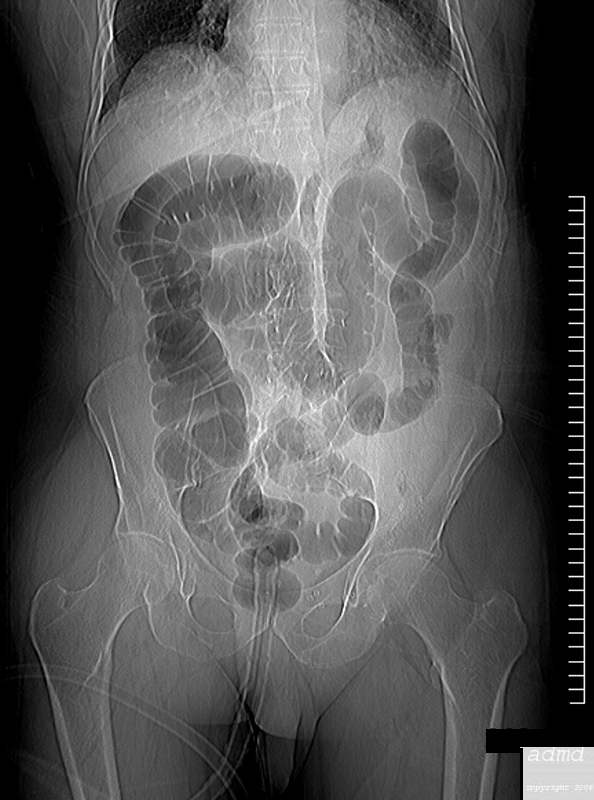 Has there Been Adequate Distension? Has there Been Adequate Distension?
Scout KUB |
| 75311 ascending colon descending colon transverse colon sigmoid size character shape folds normal anatomy Ct colonography Virtual colonoscopy CTscan scout film KUB preliminary Courtesy Ashley Davidoff MD |
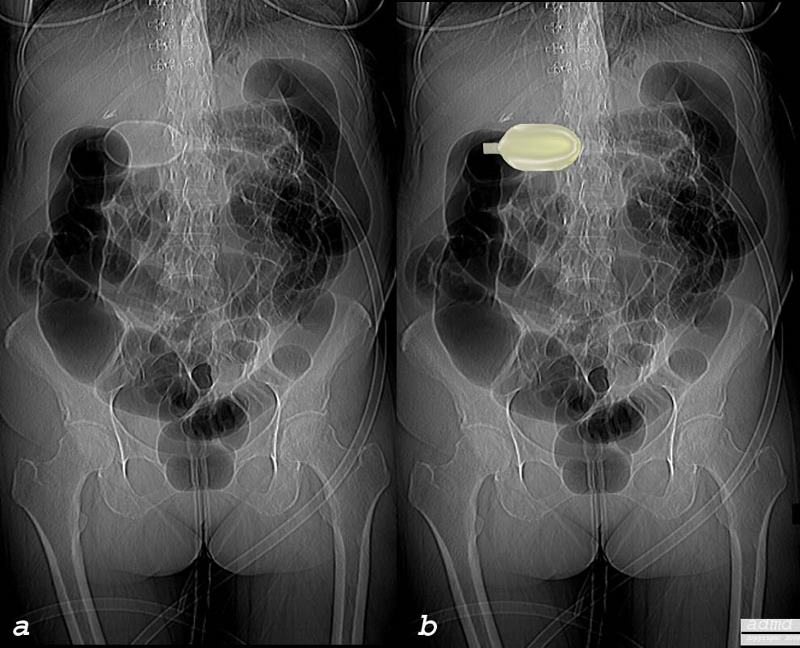 Balloon Air Insufflation Balloon Air Insufflation |
| 75449c02.800 colon large bowel air insufflation balloon puffs technique scout film CT colonography virtual colonoscopy technique CTscan Courtesy Ashley Davidoff MD Scott Tsai MD |
Data Acquisition
Supine Series
Acquisition of the CT data is next. MDCT allows for a acquisition of a large volume of data quickly, thereby reducing respiratory motion artifacts. Coverage of the abdomen and pelvis can be obtained in a single breathhold.
Axial Acquisition
For a 64 detector scanner set at 64 x 0.75 mm collimation, a breathhold of 10 seconds covering the entire abdomen and pelvis can be achieved. Using this detector configuration, thin overlapping images, near isotropic
voxels can be obtained. That means each volume or voxel of data is nearly equal in all dimensions. When voxels are non-isotropic as when data are acquired with single detector scanners, the z-direction is longer than the x and y dimensions. With MDCT voxels are near isotropic. This means that excellent quality 3D reconstructions and endoluminal fly throughs can be made.
MDCT allows use to scan faster, so a whole acquisition can be obtained in a single, short breathhold and this reduces motion artifacts.
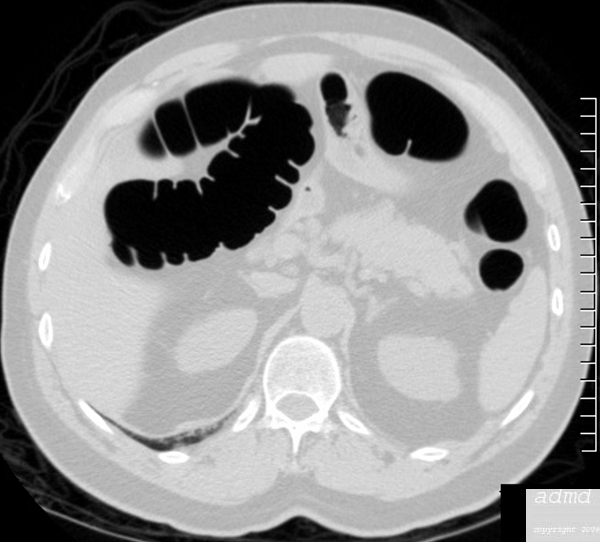 Scan in Supine and Prone Position Scan in Supine and Prone Position |
| 75295 75339 hepatic flexure splenic flexure prone large bowel normal anatomy air contrast study CT colonography virtual colonoscopy Courtesy Ashley Davidoff MD |
Scout Film Prone Series
Supine and prone acquisitions are mandatory for three reasons. First, the allows optimal distension of different segements of the colon. For example, the sigmoid colon is often poorly distended in supine especially in patients with severe diverticulosis but when prone, the sigmoid becomes non-dependent and therefore is much better distended. Second, supine and prone imaging allows any residual fluid to redistribute and unmasks any polyp that can be obscured by dependent fluid. Third, any mobile material implies stool rather than a polyp. However, this can be a pitfall.
 Prone Scout Prone Scout |
| 75435 colon distension with air tube reflux of air into terminal ileum through an incompetent ileocecal valve CT colonography virtual colonoscopy CTscan Courtesy Ashley Davidoff MD |
Axial Acquisition Prone Series
 Scan Prone Position Scan Prone Position |
| 75295 75339 hepatic flexure splenic flexure prone large bowel normal anatomy air contrast study CT colonography virtual colonoscopy Courtesy Ashley Davidoff MD |
Post Processing
After the CT data is acquired, the exam is interpreted on a dedicated workstation that allows for review of the 2D axial images, review of sagittal and coronal reconstructions and 3D views.
Whether the exam is interpreted primarily 2D with 3D for problem solving, or primarily 3D with 2D problem solving is dependent on the comfort and experience of the radiologist. Either way, whether primary 2D or 3D viewing is chosen, the secondary method of viewing is an important additional tool to problem solve. The images are so sensitive to slight regions of roughening that a small piece of debris that is 3-5mms large floating on water in the colon can be identified and needs to be looked at in multiple views to confirm its nature.
3D viewing includes volume rendering techniques such a split view (cube view), fillet view, and endoscopic fly throughs.
2D Techniques
Some radiologists will first review the axial images on the PACS station since they are most comfortable with this view, and will run through the supine view staring from the one end of the colon and continuing to the other, in both the supine and prone view and will make a note of suspicious areas and confirm the area in the other view. They will then proceed to the 3D work station and cross correlate with 3D views.
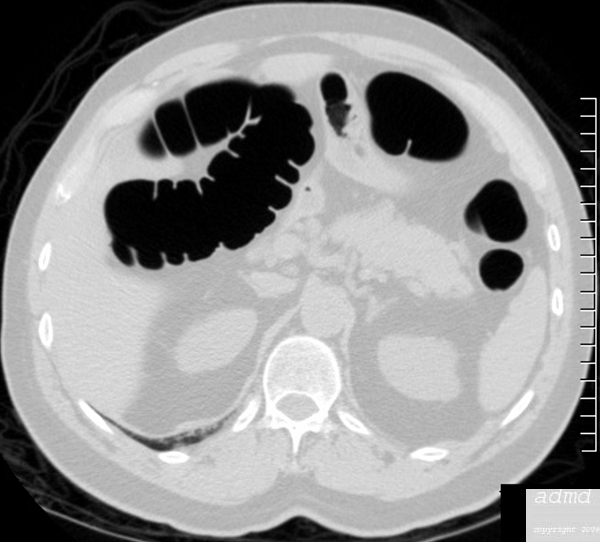  Scan in Supine and Prone Position Scan in Supine and Prone Position |
| 75295 75339 hepatic flexure splenic flexure prone large bowel normal anatomy air contrast study CT colonography virtual colonoscopy Courtesy Ashley Davidoff MD |
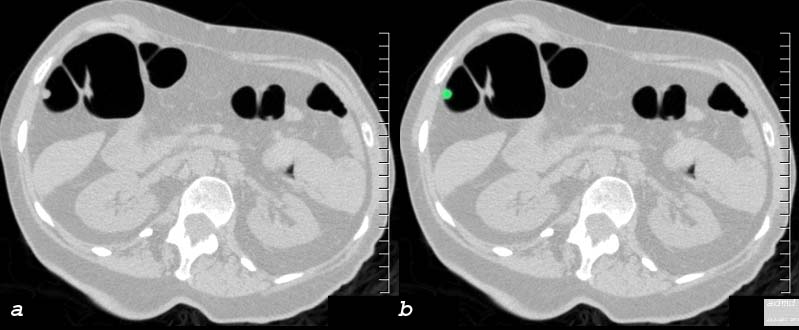 Small Polyp in the Hepatic Flexure Small Polyp in the Hepatic Flexure |
| 75370c01 ascending colon fx 6mms polyp axial images colonic folds neoplasm technique interpretation CTscan Ct colonography Virtual colonoscopy Courtesy Ashley Davidoff MD Scott Tsai MD |
3 D Viewing
Raw Data – Axial Images
The first step is to import the axial data from both the prone and supine series into the work station so that all the raw images are available for manipulation.
Define lines
The next requires a line to be drawn through the centre of the colon. This is done automatically at first and can be manipulated manually if necessary. It is drawn for both the supine and prone view.
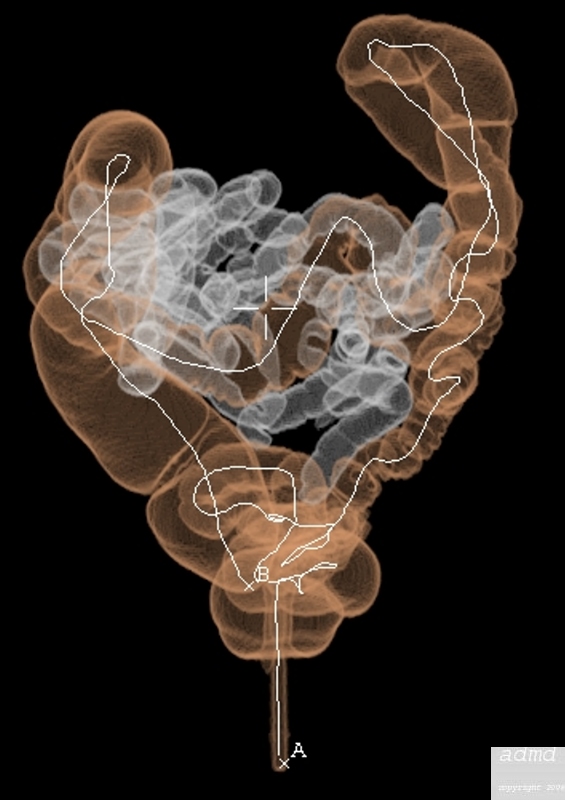
|
|
| The white line defines the colon which has been colored orange. An incompetent ileocecal valve allowed the terminal ileum to be distended with gas, and so part of the small bowel was reconstructed and appears as “white bowel” in the image, but the computer was intelligent enough not to call this colon and therefore the defining lines did not extend nto the small bowel.
75418b01 75419b01 colon define lines reflux of air through ileocecal valve Ct colonography virtual colonocsopy Courtesy Ashley Davidoff MD |
In the above instance, there had been an incompetent ileocecal valve and so part of the small bowel was reconstructed and appears as “white bowel” in the image. The computer however is intelligent enough not to call this colon and therefore the defining lines did not extend into the small bowel.
Once the radiologist or technologist is satisfied that the white line is accurately placed and in the extent of the colon, they move to the next step called “navigation”
Navigate
The radiologist can use either the fillet view or the fly through view as the primary navigation tool.
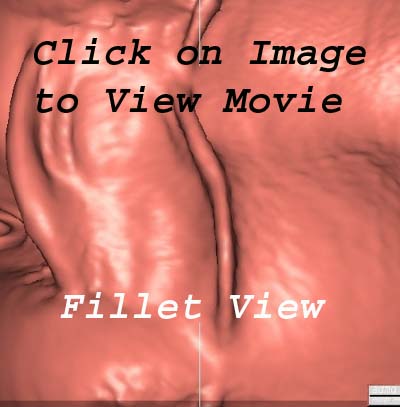
Fillet View
 Fillet View Fillet View |
| 75367b01 ascending colon hepatic flexure polyp fillet view CT colonography virtual colonoscopy CTscan 3D Courtesy Ashley Davidoff MD Scott Tsai MD |
Many radiologists prefer the fillet process since the whole colon is laid out and there is a senses that polyps and cancers have no place to hide.
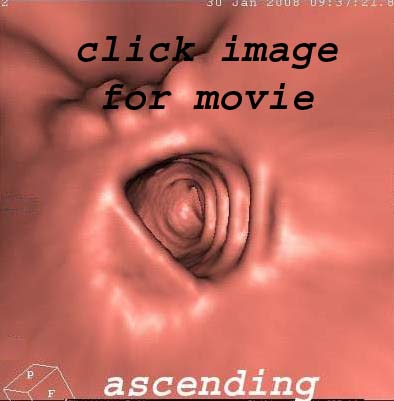
Flythrough View
The fly through is a virtual trip through the colon and is closer to the experience of the colonoscopist. There is a sense that one is forward looking and that polyps behind folds can be missed.
Fly through View Normal Ascending and Descending Colon |
| Colon Carcinoma |
| 75420b03 fly through view colon cecal carcinoma mass CT colonography virtual colonoscopy CTscan Courrtesy Scott Tsai MD |
As one proceeds with a the primary technique whether it be the fillet view or the fly through the interpreter is looking for areas of mucosal nodularity. Common artifacts along the way include debris on the surface of residual water puddles and diverticuli which can masquerade as polyps. It is thus very important to correlate the finding with other views (split view and axial view by marking the finding and cross referencing the finding on the other views which are both present on the screencan Proceed – when something is found that is questionable then
| An Observation and Cross Referencing and Cross Correlation |
| There are two rounded findings lying side by side on the fillet view. The “+” in a, marks the finding and is cross referenced with a similar “+” on the split view in b, scout view in c, zoomed axial in d, and axial view in e. In addition the split view can be rotated in order to get different perspectives of the finding. In this case the finding is a diverticulum and the interpreter would then go back to the fillet view and continue the navigation process.
75422c01 sigmoid colon fillet view split view diverticulum diverticulosis CT colonography virtual colonoscopy CTscan technique Courtesy Scott Tsai MD |
If on the other hand the finding is considered positive such as in the case below then it is marked as a “confirm finding”
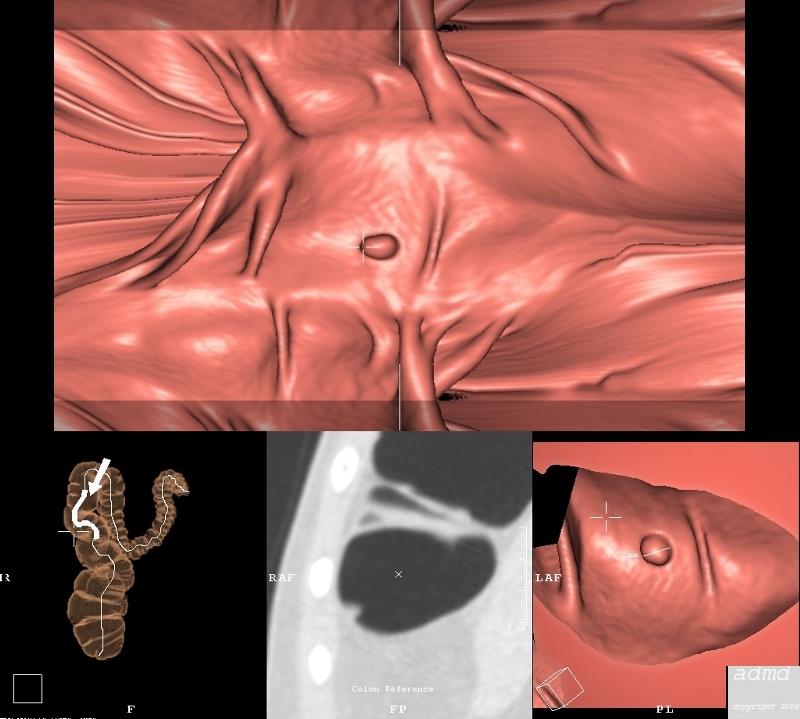 3D Reconstructions and Cross Correlations 3D Reconstructions and Cross Correlations |
| In this instance a small nodule that is about 5mm is spooted on the fillet vew (top, its position in the hepatic flexure is confirmed on the scout view, the axial view is not quite clear, but in the split or cuboid viewit is rotated and confirmed to be a small polyp.
75368.800 hepatic flexure colon large bowel fx polyp 6mm colonic folds mucosal folds 3D virtual colonoscopy CT colonography CTscan Courtesy Ashley Davidoff MD Scott Tsai MD |
One repeats the navigation process in the prone view, marking interrogating and confirming and in the end one is able to compare the two views to ensure that the interpreatations of lesions is confirmed in two views.
References
Macari, Lavelle, Pedrosa, et al
Effect of Different Bowel Preparations on Residual Fluid at CT Colonography
Radiology. 2001;218:274-277.
Aim
The aim of the procedure is to identify neoplastic colonic mucosal disease, to measure the size of the lesion, evaluate its shape, and character, and to identify its location.
| Results
The Common Vein Copyright 2008 Introduction Most studies to date have been single center in populations with high prevalence of polyps. These studies have in general yielded good results for large polyps, that is polyps greater than 1 cm, with Sn > 80% and most >90% and specificities near 90% and greater. With medium polyps 6-9mm range sensitivities drop significantly ranging from 40 to 100%. However, there are three multi-center trials to date. The most promising was Pickhardt’s prospective study in a general screening population. In fact VC had a higher sensitivity than optical colonoscopy for polyps > 1cm. There are 3 more multi-center trials in progress. Preliminary results of a multicenter trial in the US, the National CT Colonography Trial (ACRIN 6664), completed in the fall of 2007, has demonstrated excellent results, with VC Sn 90% and Sp 86% for adenomas ≥1 cm and Sn 84% and Sp 86% – 89% for lesions ≥7mm. Replication of Pickhard’t results will probably be necessary before widespread adoption of VC into general screening population. However, there are others who believe that the data already supports the addition of VC to screening program and that it would be a strong second to colonoscopy when compared with the four other current screening tests.
|
Complications
Introduction
CT colonography is a very safe test. A survey of members of the Working Group on Virtual colonoscopy in September 2005 (6) showed an overall complication rate of 0.02%, total perforation rate of 0.009% (1 of 10 962 patients) and symptomatic perforation rate (the relevant rate that can be compared with the rate of conventional colonoscopy) was 0.005% ( 1 of 21 923 patients)
Four clinically significant complications occurred, one patient with a symptomatic perforation requiring surgery, two patients with acute renal failure exacerbated by the bowel preparation and one patient who had angina.
Conclusion
Colorectal cancer is the third most common cause of cancer death in the United States and screening can reduce the rate of death (8). Standard colorectal cancer screening methods include colonoscopy , double contrast barium enema, flexible sigmoidscopy and fecal occult blood testing. Despite many studies showing the efficacy of CT colonography, the procedure is still not reimbursed by Medicare and other third party payers, nor has it been incorporated into colorectal cancer screening guidelines.
Advocates of CT colonography however note that it is gaining favor as an effective screening test from the American Cancer Society and the National Cancer Institute and predict that it will soon gain Medicare approval. This will lead CT colonography to become a radiologic practice standard, especially with less than 50% of eligible Americans being screened (9).
The key for CT colonography is quality in all key areas of performing an optimal test, particularly, bowel preparation, colonic distention, MDCT scanning and image interpretation (9). When performed properly, CT colonoscopy is an effective test for detecting clinically significant colorectal polyps and “may have a profound effect on screening for and prevention of colorectal cancer.” (7)
References
- Channin DS. Lumina, voxels, and bits: update on virtual reality imaging. Appl Radiol 1997; (suppl):51-4.
- 1. Vining DJ, Gelfand DW, Bechtold RE, et. al. Technical feasibility of colon imaging with helical CT and virtual reality (abstr.) AJR Am J Roentgenol 1994; 162(Suppl 1):104.
2. Johnson CD, Dachman AH. CT Colonography: The Next Colon Screening Examination? Radiology. 2000; 216:331-341
3. Pickhardt PJ, Choi R, Hwang I, Butler JA, et. al. Computed Tomographic Virtual Colonoscopy to Screen for Colorectal Neoplasia in Asymptomatic Adults. N Engl J Med 2003; 349:2191-2200.
4. Johnson CD, et. al. Prospective Blinded Evaluation of Computed Tomographic Colonography for Screen Detection of Colorectal Polyps. Gastroenterology 2003; 125: 311-319.
5. Cotton PB, et. al. Computed tomographic colonography (virtual colonoscopy) -a multicenter comparison with standard colonoscopy for detection of colorectal neoplasia.
JAMA 2004; 291:1713-1719.
6. Pickhardt PJ, Barish MA, Barlow DS, et. al. Significant complications at CT colonography: survey results from the Working Group on Virtual Colonoscopy. Sixth International Symposium on Virtual Colonoscopy, Boston, Mass, October 17-18, 2005.
7. Pickhardt PJ. Screening CT Colonography; How I Do It. AJR 2007; 189:290-298.
8. Ransodoff DF, Sandler RS. Screening for Colorectal Cancer. N Engl J Med 2002; 346: 40-44.
9. Boshamer C (editor). CTC is Hot…and is about to get hotter. In Practice Quarterly Publication of the ARRS. 2008; 2:5-7.


 Defining the Lines
Defining the Lines