Imaging the Colon
The Common Vein Copyright 2007
Introduction
The plain film of the abdomen was the initial study that enabled physicians to study the colon after Roentgen discovered X-Rays in 1898, while barium sulphate as a contrast agent in the intestinal tract was first used by Krause in 1910. (Schott) The plain film still remains the study of choice for patients suspected of having acute colonic disease in the emergency room, particularly when bowel obstruction, volvulus, ischemia, or bowel perforation is suspected. Prior to colonoscopy, use of the single contrast barium enema, followed by double contrast barium, were the only methods available for the diagnosis of mucosal disease. With the development and refinement of colonoscopy starting in the 1950’s, it is now the procedure of choice to study the mucosa since it not only allows direct visualization, but also provides an opportunity to intervene if necessary. The concept of “point of care” is an important evolving concept in medicine and relates to the timely relationship between diagnosis and treatment. The closer in time that accurate diagnosis, and successful treatment can come, the more valuable the care. In the case of colonoscopy, the ability to first diagnose an abnormality and then move forward with either a biopsy for definitive diagnosis, or definitively treat a small a small polyp or bleeder at the same sitting for example, make this a valuable “point of care” tool. It is however a procedure that usually requires sedation, carries a small risk of perforation (0.2-0.4% with diagnostic colonoscopy and 0.3-1.0% with polypectomy). (eMedicine)
Full visualization of the colon is not always accomplished by colonoscopy due to redundancies or severe obstruction. Colonoscopy requires insufflation of air so that in patients with severe inflammation or a weakened wall the risk of rupture or translocation of organisms into the circulation is limiting, and therefore the procedure is relatively contraindicated in these conditions. Lastly colonoiscopy is a technique that is focused to the mucosa of the bowel and is not able to evaluate the deeper layers. Conventional CT on the other hand is able to evaluate the wall of the colon and also allows a global view of the abdomen. Identifying small polyps and sometimes even large mucosal masses is not consistently within the realm of conventional CT for a few reasons, but mostly due to the presence of feces, and the variable degrees of distension and non distension of the bowel which can mask soft tissue changes like a mass. CT colonoscopy is a study of the clean colon with the use of air to distend the colon. This allows the radiologist to evaluate the mucosa, and polyps as small as 5mms can be identified. In patients who have had a failed colonoscopy it is the study of choice. It is not uncommon to have a patient transported to CT from the endoscopy suite, to complete a colonoscopic study because the endoscopist had failed to traverse a redundant colon or a severe obstruction. Despite its strength to evaluate the wall it cannot differentiate the layers of the wall as well as ultrasound or MRI. These studies are limited at this time to the rectal wall only, but their ability to define the layers is exquisite and they play a very important role in the staging of rectal cancer by defining the extent of tumor penetration into, and sometimes through the wall. The depth of tumor penetration has bearing on how a tumor will be treated. In order for the US or MRI to obtain the necessary resolution the probes have to be in close contact with the mucosa, limiting the techniques at this time to the evaluation of the rectal wall.
PET-CT has been an extremely valuable addition in the management of cancer in general, but in the colon has found specific applicability in staging the disease and for detecting recurrence.
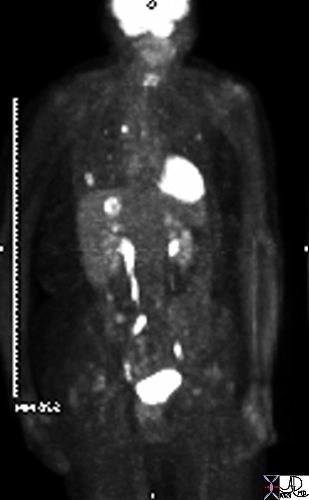
PET for staging sigmoid carcinoma |
| In this elderly female with known sigmoid colon carcinoma, the PET CT is positive for metastatic disease in the liver, lungs, and mediastinum. The findings include high FDG uptake in a single focus in the dome of the right lobe of the hepatic parenchyma, as well as in multiple small foci in both lungs, and a single very bright focus in the mediastinum. These findings reflect stage IV disease.
Ashley Davidoff MD 45132 |