Benign Polyps of the Colon
The Common Vein Copyright 2008
Definition
Colonic polyps are growths of the of the colonic mucosa with multiple causative associations. They are common (30-50% of the adult population), often linked to the aging process, diet, and sometimes are associated with a genetic predispostion.
The resulting lesion is structurally characterized as a nodule or mass that extends from the mucosa of the colon into the lumen, either with a stalk (pedunculated) or with a flat base (sessile). They usually have no functional implications.
At the histopathological level, three basic benign types of polyps exist. Hyperplastic polyps represent an overgrowth of normal mucosa, and the resulting nodule remains under the regulatory processes of the body. They are considered to be a physiological response to an environmental stimulus. These are the most common type of polyp. Adenomatous polyps are true neoplastic lesions of the mucosa, and represent a pathological process, where the resulting cell mass is not under the normal regulatory mechanisms of the body. Adenomatous polyps are benign but are considered precursors to cancer of the colon. The third group of polyps are hamartomas which represent disorganized mucosal elements that also present as a polyp. A miscellaneous group of polypoid like lesions include inflammatory polyps, pseudopolyps and lymphoid polyps. Submucosal lesions such as carcinoid mass, lipomas amd leiomyomas arise from the submucosa and hence may masquerade as mucosal lesions as they push into the lumen.
Structurally polyps may be sessile or pedunculated. The histological characteristics enable stratification into the categories of hyperplasia, adenomatous, and hamartomatous. The association with malignancy is a concern for all polyps that are adenomatous and hamartomatous. There are rare instances were hyperplasstic disease is associated with malignancy.
Polyps do not usually affect colonic function except when complicated for example by causing intussusception, which results in intermittant obstruction and in the more severe cases can cause obstruction and even ischemia.
About 1% of all polyps are complcated by malignant change. Adenomatous polyps are considered a precursor to malignancy. Transformation of hamartomatous lesions into malignant disease also occurs but is less common than the occurrence with adenomatous polyps.
Polyps are most commonly diagnosed initially by the endoscopist and the histology documented by the pathologist. CT colonography and barium are second line diagnostic methods.
Polyps under 2cms are usually treated at the time of endoscopy by polypectomy, and larger lesions are treated with surgery.
 5mm benign polyp – path specimen 5mm benign polyp – path specimen |
| This 5mm polyp is a common finding on colonic evaluation and at this size is a benign abnormality. Left intact it can grow into a monster. Hence it is usually removed by the endoscopist.
Courtesy Ashley Davidoff MD 12087
|
Principles
Histology
The first step in understanding polyps is to explore the normal histology of the colon. Like many other tubes in the body its wall has 4 layers. The inner layer, the mucosa is the origin of all polyps and it on a basement membrane. The mucosa consists of a single layer of rectangular cells and the layer is called an epithelium. Because of the rectangular shape of the cells they are called columnar cells and so the layer is called a columnar epithelium. The second layer is the submucosa which contains blood vessels, lymphatics, nerves and loose connective tissue. The third layer is the muscular layer called the muscularis and the fourth layer is called the serosa or adventitia which acts as a protective outer “skin” for the colon. This layer is called a serosa when it is surrounded by peritoneum (transverse colon and sigmoid colon) and called an adventitia when it is retroperitoneal. (ascending colon, descending colon and part of the rectum)
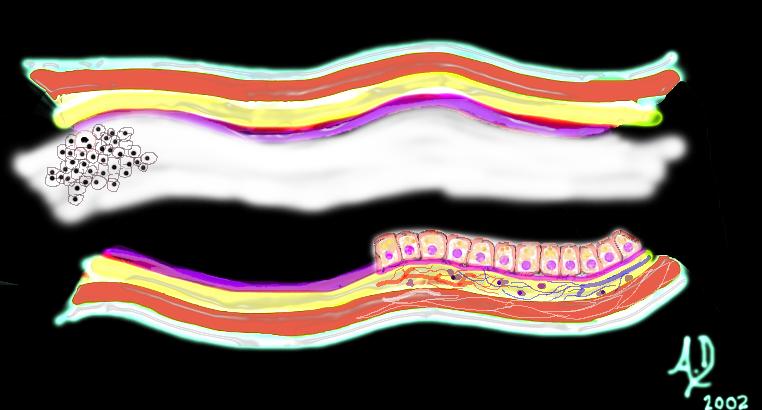
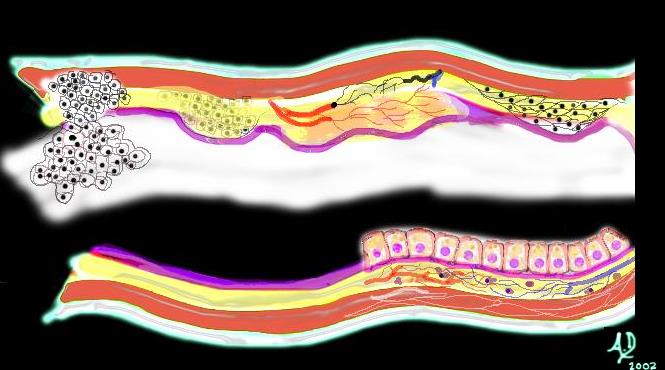
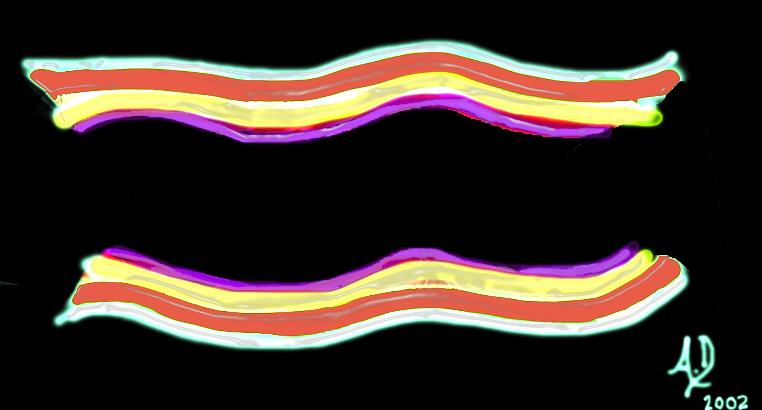 The 4 basic layers of the colon The 4 basic layers of the colon |
| This diagram illustrates the 4 basic layers of the colon. The inner pink layer is the mucosa, the yellow layer beneath the mucosa is called the submucosa, while the red layer is the muscular layer (muscularis) and the 4th layer is called the serosa or adventitia.
Courtesy Ashley Davidoff MD 32338 |
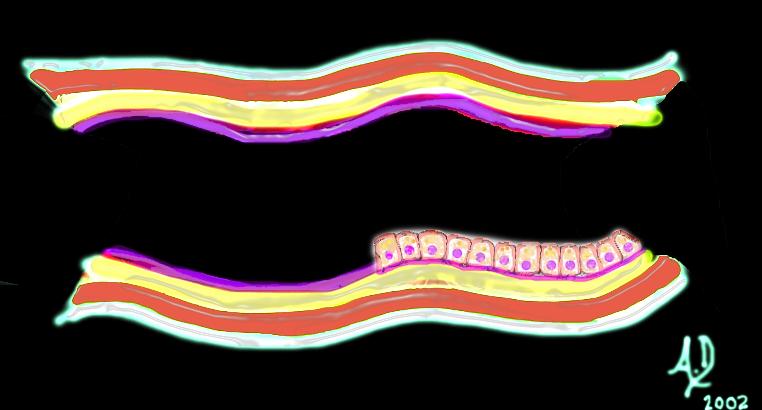 The mucosa The mucosa |
| The mucosa consists of a simple columnar epithelium which means it is a single layer of epithelial cells that are each shaped like a column – similar to a tall rectangular block of apartments.
Courtesy Ashley Davidoff MD 32347 |
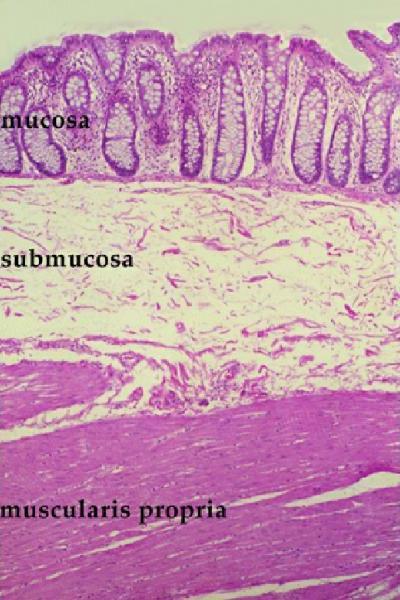 Histology of the mucosa, submucosa and muscularis Histology of the mucosa, submucosa and muscularis |
| The histological section shows three of the four layers of the colon – mucosa on the luminal side, submucosa of loose connective tissue and the muscularis. Note how the mucosa is thrown into folds of tightly packed crypts resembling a line of test tubes.
Courtesy Barbara Banner MD 12047 |
 Normal Colonic Mucosa Normal Colonic Mucosa |
| This is a low power photo micrograph of normal colon mucosa illustrating extremely orderly, rigid, “test tube”-like arrangement of the straight tubular glands which comprise the colonic crypts.
Courtesy Barbara Banner MD 12860 |
Principles of Disease
The mucosa is a highly active structure and cell turnover is rapid, with the reproduction of new cells and death of old cells occurring about every four days. A variety of environmental stimuli including diet, smoking, obesity, and genetics that may stimulate the mucosa to overgrowth. The overgrowth may take the form of a physiological response (hyperplastic polyp) or a pathologic neoplastic response (adenomatous change), and sometimes are a manifestation of genetic aberrations.(adenomatous and hamartomatous polyps)
Polyps occupy space, they grow with time. Hyperplastic polyps are the most common form of colonic polyps, are usually small, round, commonly positioned in the rectum, and may take on the hue of the epithelium, or may differ. They are usually less than 6mm, but if they grow larger then associated neoplasia must be sought. Adenomatous polyps are usually diagnosed when they are in the 3-5mm range and about 1% will become malignant 10 to 15 years later. Since they occur in a capacious space they do not affect function and are generally asymptomatic.
Size and histological type are important considerations in the diagnosis and treatment of polyps. As the polyp enlarges the chances of malignancy increase.As stated above, a polyp that is greater than 1.5cms in size starts to be of concern.
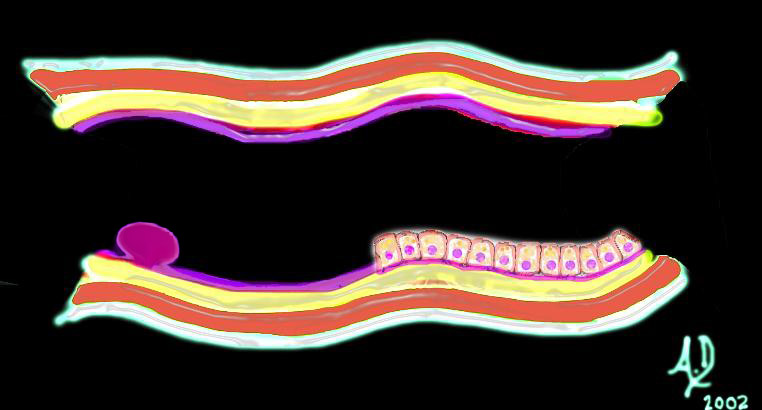
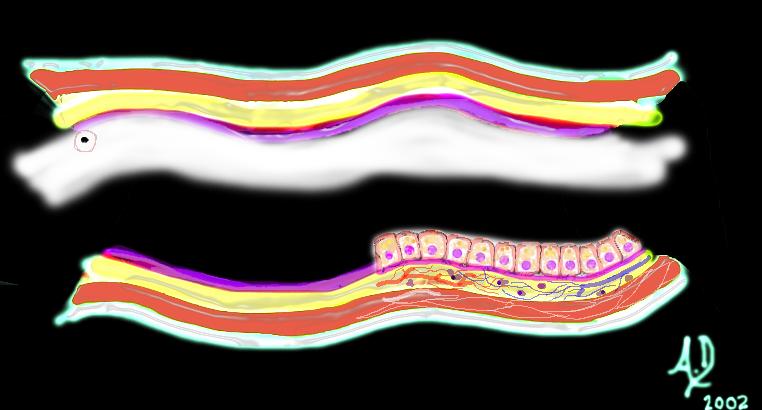 Mucosal disease –beginning of a neoplasm Mucosal disease –beginning of a neoplasm |
| The diagram shows a single columnar cell on the top side of the lumen that for whatever reason has been programmed to become “different” and instead of growing with characteristic columnar shape with pink nucleus and “peaches and cream” cytoplasm in this case has become round with white cytoplasm and black nucleus. It is a neoplasm – ie a new growth.
Courtesy Ashley Davidoff MD 32354 |
 Mucosal disease -neoplasm Mucosal disease -neoplasm |
| Over time this neoplasm will continue to grow. If it grows slowly with monotony and uniformity in the morphology of cells, minding its own business and not disturbing its neighbors it is considered a benign neoplasm. It would be called a benign polyp and since it arises from the mucosa, it would be called an adenomatous polyp.
Courtesy Ashley Davidoff MD 32355 |
Principles in Imaging
The polyp is seen as a nodule on the surface of the bowel and because it arises from the mucosa the angles created with the mucosa are acute.
 Mucosal Lesion Acute Angles with the Surface Mucosa Mucosal Lesion Acute Angles with the Surface Mucosa |
| 32347d01 mucosa submucosa muscularis adventitia serosa mucosal mass polyp neoplasm carcinoma acute angles with the lumen histopathology imaging diagnosis Davidoff art Davidoff MD |
Diseases that affect the submucosa such as edema, or hemorrhage, or inflammation cause a heaping up of the mucosa, and the shape of a submucosal lesion is quite different. It is seen by the endoscopist, or double contrast enema as a heaped up lesion with obtuse angles. Lesions of the submucosa may occur in acute inflammatory or ischemic diseases, or in neoplastic diseases such as lymphoma or lipomas. Lesions arising from the muscularis, such as leiomyomas also create an obtuse angle (and sometimes a right angle with the mucosal surface.
 Submucosal Lesion Obtuse Angle or Right Angle Submucosal Lesion Obtuse Angle or Right Angle
Lesion Arising From the Muscularis – Obtuse Angles |
| 32347d02 32347d03
mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage obtuse angles or right angle 90 degree ninety degree angle with the lumen histopathology imaging diagnosis Davidoff art Davidoff MD |

5mm benign polyp |
| This 5mm polyp is a common finding on colonic evaluation and at this size is a benign abnormality. Left intact it can grow into a monster. Hence it is usually removed by the endoscopist.
Courtesy Ashley Davidoff MD 12087 |
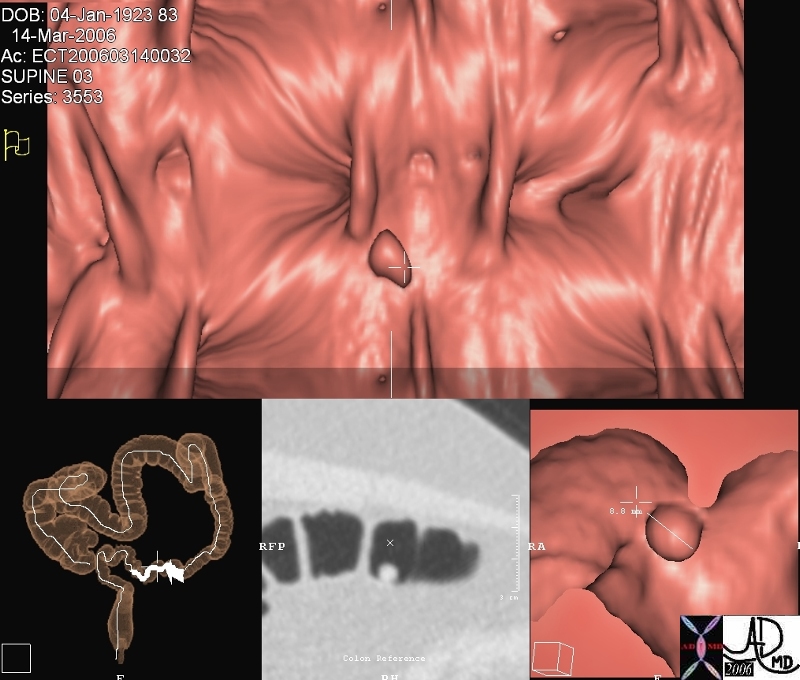
Benign Polyp – virtual colonoscopy
This series of images from a virtual colonoscopy shows an 8 mms polyp seen on the surface rendering images (salmon colored images) referenced to the sigmoid colon (bottom left) and with conventional CTimaging (bottom middle) At this size the polyp is almost certainly benign and can be removed through the colonoscope safely. Note in the gray scale image (middle image 2nd row) the acute angles formed by the polyp with the underlying mucosa. The distal location raises the likelihood that it represents a hyperplastic polyp.
Courtesy Scott Tsai MD
45119
Causes and Predisposing Factors
Epidemiologic studies would favor that environmental factors play an important role since geography seems to have distinct patterns of disease. Hyperplastic polyps in Western culture may be as common as 70% of the population whereas it may only be found in 2-3% of the population in developing countries. Thus factors of importance in their development seem to include a diet that is high in fat, low in fiber, and red meat. Obesity, alcohol intake and smoking have also been implicated.
The genetic syndromes associated with polyps and their relationship to colon cancer has been significantly advanced, particullrly related to the familial syndromes including familial adenomatous polyposis. The genetic associations with the hamartoma groups of diseases are also evolving and becoming established.
Result
Pathology
There are a few different types of polyps as noted pathologically. Polyps in general start as sessile lesions and may become pedunculated.
 Sessile Polyps Sessile Polyps |
| 00360 colon large bowel mass polyp multiple polyps grosspathology Courtesy Barbara Banner MD |
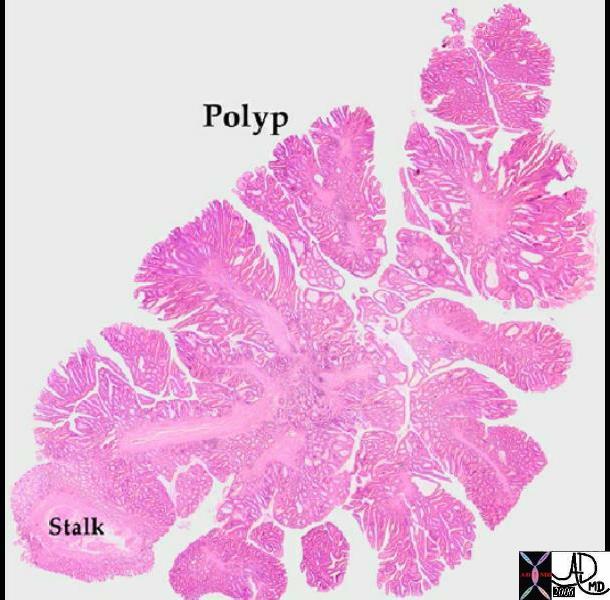
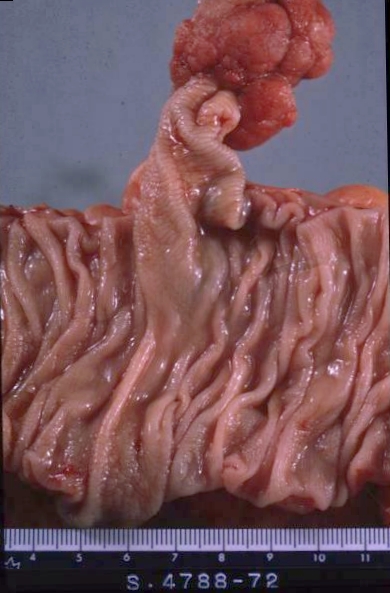 Pedunculated Polyp Pedunculated Polyp |
| 02328 colon large bowel pedunculated polyp + mucosal stalk grosspathology |
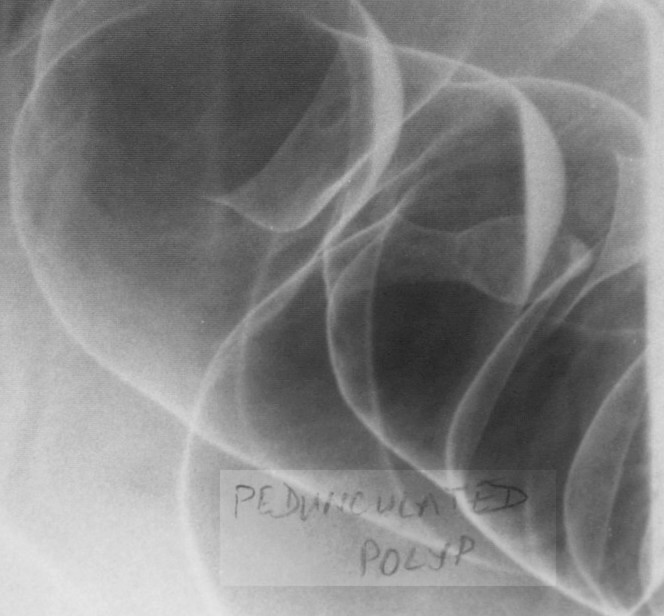 Pedunculated Polyp Pedunculated Polyp |
| 12011b colon large bowel fx pedunculated polyp fx mass dx polyp BE barium enema Courtesy Ashley Davoidoff MD 5star |
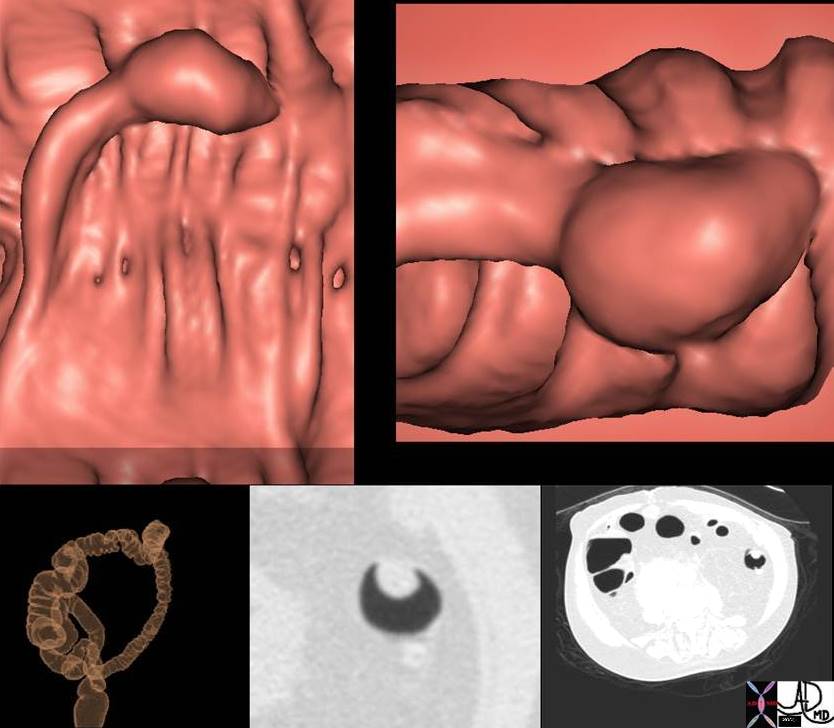 Pedunculated Polyp Pedunculated Polyp |
| 744800 colon mass polyp pedunculated polyp CTscan surface rendering 3D Courtesy Scott Tsai MD |
Hyperplastic Polyps
A hyperplastic polyp is a proliferation and overgrowth of normal mucosal cells, and is characterized as a small sessile lesion, commonly located in the distal sigmoid and rectum. It is the most common polyp in the colon and represents about 70-90% of polyps identified. They are usually the same color or perhaps lighter than the surrounding mucosa. The hyperplastic polyps are usually small (<6mm) and have no macroscopic features that would enable the endoscopist to distinguish them from adenomatous polyps. Their cause likely relates to diet and environmental factors, since they are commonly seen in Western cultures, and as small lesions, they have no definite known malignant potential. They are usually diagnosed histologically after removal at colonoscopy, and are thus coincidentally treated.
  Nomal (left) and Hyperplastic Polyp (right) Nomal (left) and Hyperplastic Polyp (right) |
| The left image shows a normal colonic mucosa. This is a low power photo micrograph of normal colon mucosa illustrating extremely orderly, rigid, “test tube”-like arrangement of the straight tubular glands which comprise the colonic crypts. The right image shows a photomicrograph at low power, showing a hyperplastic polyp of the colon. The characteristic histology is simply hyperplasia of the epithelium of existing crypts with infoldings, creating a “sawtooth” pattern in the epithelium. These polyps are typically 2 or 3 mm in diameter. colon large bowel fx polyp fx sawtooth pattern fx hyperplasia dx hyperplastic polyps histopathology Courtesy Barbara Banner MD 12307b01 |
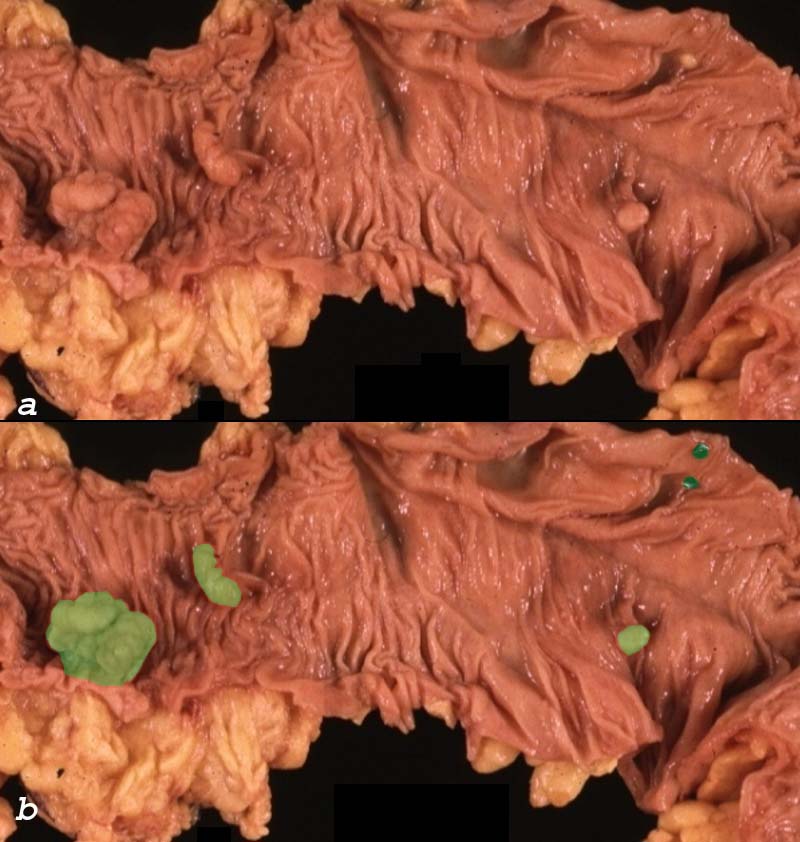 Multiple Polyps Multiple Polyps |
| This path specimen shows five polyps on the surface of the colonic mucosa. Based on the size and lobular surface, it is very likely that the polyps overalid in light green are adenomatous polyps and are likely to be tubular adenomas. The polyps overlaid in dark green , one being the same color of the mucosa and rthe second lighter than the mucosa could represent hyperplastic or adenomatous polyps. Their size smoothness and color would favor hyperplastic polyps but their location in the transverse colon would favor adenomatous polyps. Histological examination is essential to make the distinction.
00362c02 colon large bowel mass polyp multiple polyps adenomatous polyps hyperplastic polyps grosspathology Courtesy Barbara Banner MD Ashley Davidoff MD |
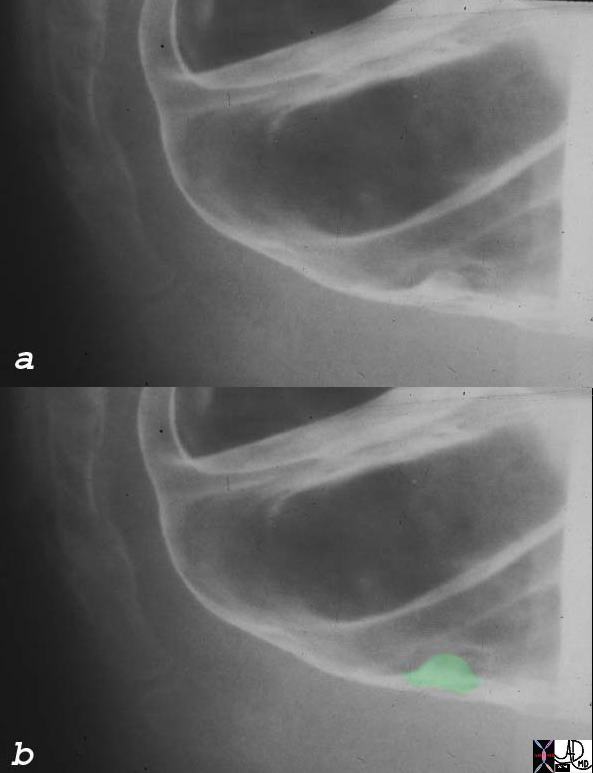 Small Rectal Polyp Small Rectal Polyp |
| This 5mm rectal polyp likely represents a hyperplastic polyp based on its size location, and the relative frequency of hyperplastic polyps in general.
00363c01 colon large bowel rectum fx nodule dx rectal polyp likely hyperplastic polyp BE barium enema Courtesy Ashley Davidoff MD |
Adenomatous Polyps
An adenomatous polyp is a benign neoplastic proliferation of mucosal cells with multifactoroal causes including a diet, obesity, smoking and genetics and the resultingadenoma is a pathological process that has a propensity to evolve into a malignant lesion over 10-15 years. When the lesions are less than 1.5cms malignancy is distinctly uncommon. As they increase in size beyond this size, the chances of malignancy increase. The lesion is diagnosed histologically after removal at colonoscopy, and is thus coincidentally treated. A follow up colonoscopy is recommended 3-5 years later.
Adenomas are characterized histolgically by a dysplastic epithelium. They show enlarged, elongated hyperchromatic nuclii that may be stratified within the cell. Mucus may or may not be present.The adenomatous polyps may be tubular, tubulovillous, and villous. The tubular adenomas are most common (70%), while the tubulovillous (20%) and villous (10%) are less common. They are often polypoid but may be flat. The flat lesions are most characteristic of the villous adenoma.
Tubular Adenoma
Tubular adenomas tend to be round and relatively smooth with lobular components divided by clefts. They are red or darker than surrounding mucosa. The adenomatous tissue proliferates in a tubular formation and hence the name. Some lesions have villous elements. If 75-80% of the lesion is tubular then it is called tubular, and similarly if it is 75-80% villous it is called a villous adenoma. A combination of the two with either represented by less than 70% make the lesion tubulovillous.
When the adenomas are less than 1cms, 90% are tubular. When they are larger than 2cms 50% are tubular, 40% are tubulovillous and 10% are villous.
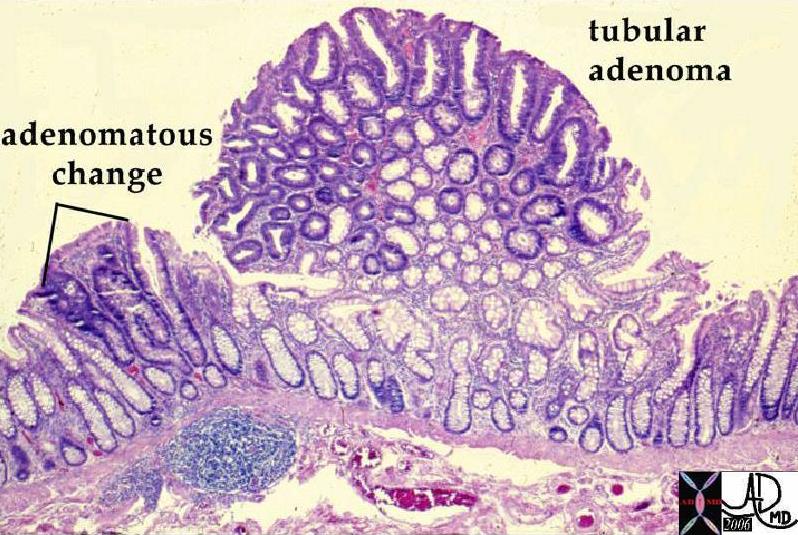 Tubular Adenomat Tubular Adenomat |
| The low power microscopic image shows a sessile tubular adenomatous polyp. Normal mucosa is seen to the right side of the image while the adenomatous polyp is seen with more blue and purple as a result of larger nuclii. At higher power, no malignant features were seen. The broad base of the polyp is a feature of a sessile polyp. The rounded nature of the tubular glands is characeteristic.
12178 colon large bowel fx mass fx polyp polypoid mass dx benign tubular adenoma dx multiple polyposis histopathology mount Courtesy Barbara Banner MD ask
|
 Adenomatous Polyp Adenomatous Polyp |
| The dark red color of the 2.5cms pedunculated polyp is more reminiscent of an adenomatus polyp and likely represents an adenomatous polyp with the associated lobulations.
12132 colon large bowel fx polyp fx stalk grosspathology Courtesy Barbara Banner MD
|
 Sessile Polyps Sessile Polyps |
| Gross pathology specimen of two polyps lying side by side. The presence of the fissures, lobularity and relatively smooth surface favors a tubular adenoma.
00360 colon large bowel mass polyp multiple polyps grosspathology Courtesy Barbara Banner MD |
Tubulovillous Adenoma
  Tubulovillous Adenoma Tubulovillous Adenoma |
| Macroscopically the distinction between the tubular adenoma and tubulovillous adenoma is difficult and the histological features would confirm that types.
12144 12147 colon large bowel fx mass fx polyp polypoid mass dx tubulovillous adenoma grosspathology Courtesy Barbara Banner MD |
 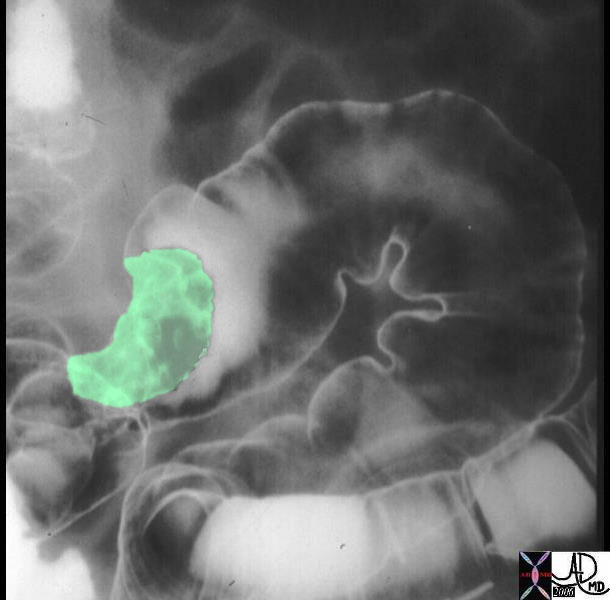 Irregular Mass is seen in the Sigmoid colon outlined by Air and Contrast of the double contrast enema. Irregular Mass is seen in the Sigmoid colon outlined by Air and Contrast of the double contrast enema. |
| The double contrast barium enema shows a large irregularly shaped mass in the sigmoid colon. The mass seen in green in the second image is greater than 2cms in size, so that the risk of malignancy is substantially increased. The fissures filled with barium is a feature of tubular adenoma, but this in the end is not a helpful criterion. more importantly the large size causes concern for malignant potential and it must be removed surgically.
Courtesy Ashley Davidoff MD 12175 12175bo1 |
Villous Adenoma
Villous adenomas have a shaggy surface with papillary fronds and tend to be flatter lesions.
They have a greater propensity to become malignant. Invasive cancer is seen in about .5% of adenomas less than 1cms, 5% in the adenomas that range in size from 1-1.9cms, and in 10% that are greater than 2cms. One third of patients with have benign disease benign, one third have carcinoma in situ, and one third will demonstrate invasive carcinoma.
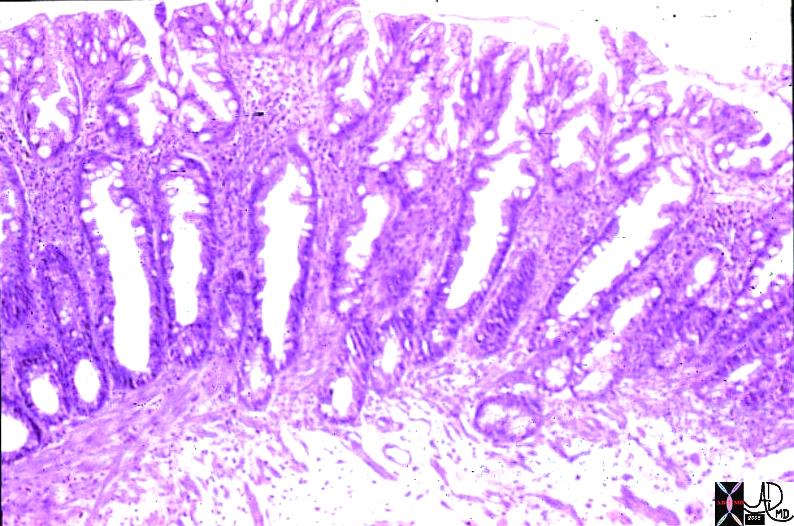
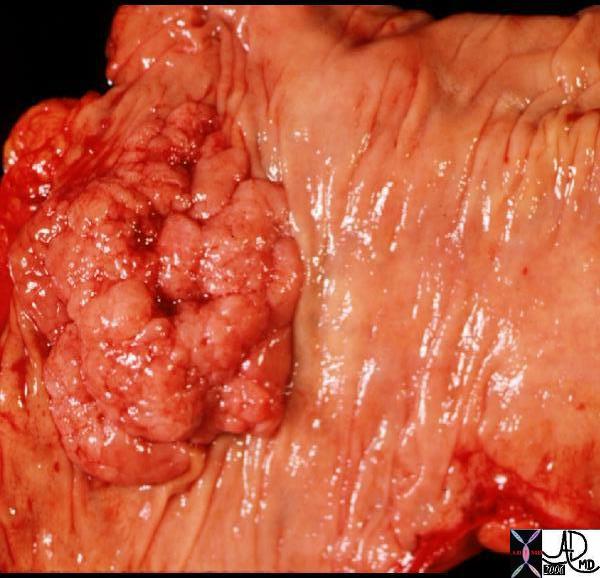 Villous Adenoma Villous Adenoma |
| The broad based polyp with fissures looks more like a tubular adenoma but it turned out to be a villous adenoma. The histopathology is not from the same patient but shows the histopathological equivalent of the characteristic papillary fronds. The barium enema on the other hand is from the same patient.
12113 colon large bowel sigmoid colon fx mass fx polyp polypoid mass dx villous adenoma grosspathology Courtesy Ashley Davidoff MD see imaging 12112
|
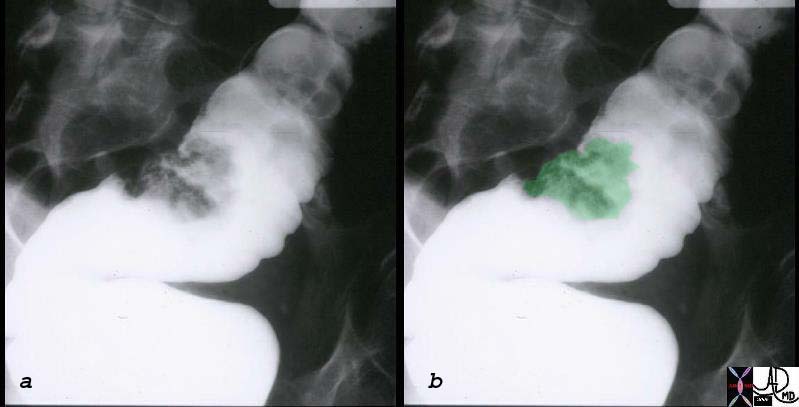 Villous Adenoma of the Sigmoid Colon Villous Adenoma of the Sigmoid Colon |
| The single contrast barium enema shows a sessile mass that is in the 2-3cms range. The gross pathological specimen is noted above and at pathology was shown to be a villous adenoma.
12112c01 colon large bowel sigmoid colon fx mass fx polyp polypoid mass dx villous adenoma BE barium enema Courtesy Ashley Davidoff MD see pathology 12113 |
Familial Adenomatous Polyposis
Definition
Familial adenomatous polyposis (FAP) is the most common adenomatous polyposis syndrome, and it is characterized by the presence of innumerable neoplastic tubular adenomatous polyps of the colon. The cause of the disease relates to an autosomal dominant inherited disorder. In early life (about 16 years) the genetic defect evolves into and results in a colonic mucosa that is carpeted with hundreds to thousa
nds of adenomatous polyps. In 100% of patients the syndrome is complicated by the development of cancer at the age of 30 – 40 and hence all patients should be treated with colectomy in early years of the disease. (teenage to early 20’s)
Associated diseases include desmoid tumors (4-30%) and other rarer associations including medulloblastoma, thyroid cancer, adrenal cancer, gastric cancer and pancreatic cancer.
The diagnosis is established in patients who have a positive family history and by colonoscopy demonstrate more than 100 polyps.
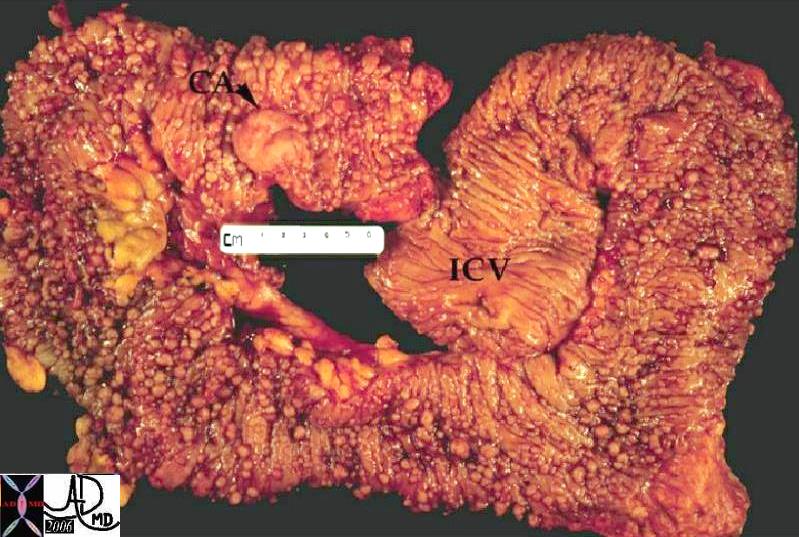 Familial Polyposis Syndrome with Carcinoma Familial Polyposis Syndrome with Carcinoma |
| The normal mucosa in this patient has been replaced by inumerable carpet of polyps extending throughout the colon. A malignancy has evolved (“ca” = carcinpoma) at the distal end of the colon. |
Clinically it is usually asymptomatic and only presents presents once the patient has developed cancer. Symptoms include abdominal pain, diarrhea, mucus diarrhea, and bloody diarrhea.
Colonoscopy is the imaging and diagnostic study of choice since the diagnosis can be established and biopsy of suspicious lesions can be accomplished.
Colectomy with mucosal proctectomy and ileoanal pouch pull-through is the therapeutic procedure of choice
References
eMedicine Familial Adenomatous Polyposis
Peutz-Jeghers syndrome
Peutz-Jeghers syndrome
Definition
Peutz-Jeghers syndrome is an autosomal dominant inherited disorder of the intestinal tract characterized by by intestinal hamartomatous polyps associated with mucocutaneous melanocytic macules typically seen around the mouth.
The entity is caused by a gene mutation resulting in hamartomas most commonly seen in the small bowel but also in the colon and the stomach, and can be complicated by intestinal intussussception and carcinoma (15 fold increase). Risks of carcinoma in order of relative risk are small bowel, stomach, pancreas, colon, esophagus, ovary, lung and breast.
The diagnosis is suspected clinically when family history of the disease is present, and melanocytic lesions (freckles) seen on the face, around the mouth and on the buccal mucosa. Histologically the polypoid lesions shows proliferation of smooth muscle throughout the polyp.
Imaging includes the use of colonoscopy, small bowel follow through, enetroclysis and videocapsule imaging.
Treatment options depend on the extent of the polyps. If accessible to eneteroscopic polypectomy this should be performed. In patients with intusussception or when malignancy is suspected, surgery is iindicated.
The entity was first described by Peutz in 1921 who recognized the syndrome in a Dutch family, and further descriptions by Jegher in 1940 helped consolidate the syndrome.
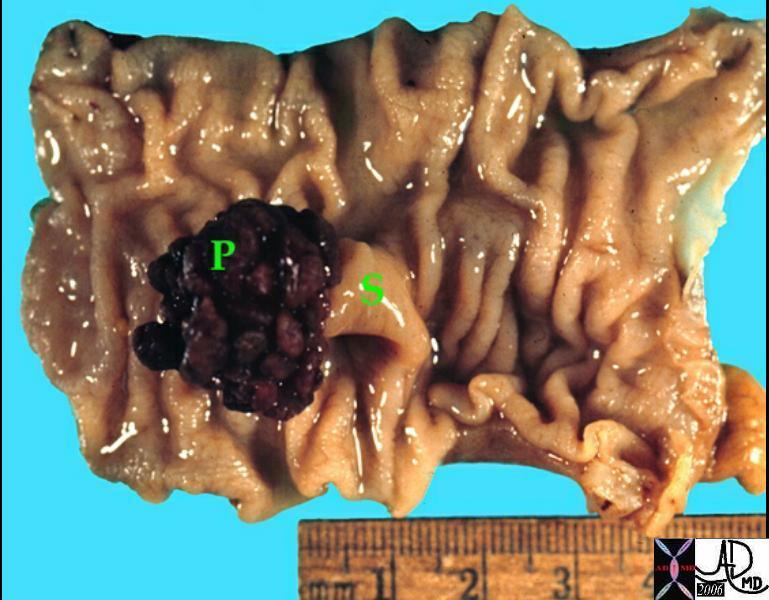
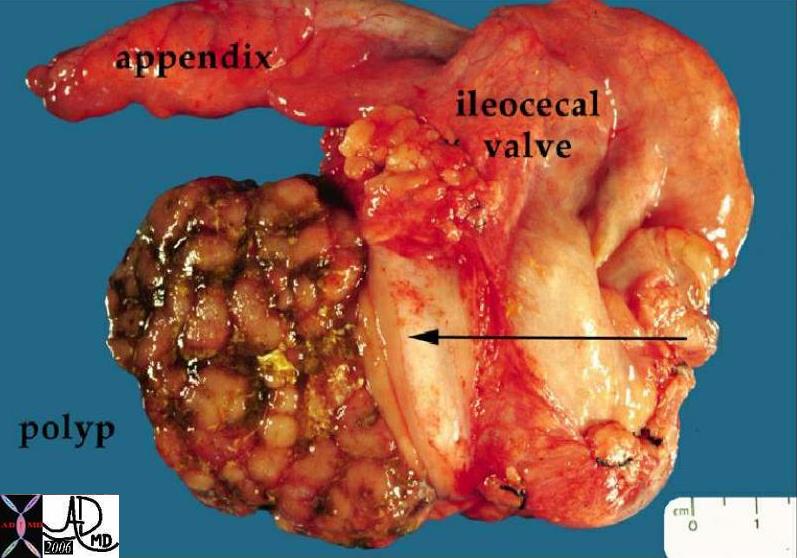 Peutz-Jeghers Syndrome Peutz-Jeghers Syndrome
Hamartomatous Polyp in the Cecum |
| 12190 colon large bowel cecum fx mass fx polypoid mass dx Peutz-Jegher’s syndrome Peutz-Jeghers syndrome grosspathology Courtesy Barbara Banner MD ask |
 Hamartomas in the Small Bowel – Peutz-Jeghers Syndrome Hamartomas in the Small Bowel – Peutz-Jeghers Syndrome |
| Young male with buccal melanocytic lesions presents with intermittant colicky abdominal pain. The filling defects seen in the small bowel (green) are consistent with polyps. There is also a loop of small bowel in the right upper quadrant that is dilated. These findings are consistent with hamartomas in the small bowel in a patient with Peutz Jegher’s syndrome and intusussception should be considered.
00511c01 small bowel dx intussusception fx polyps dx Peutz- Jeghers upper GI UGI imaging radiology contrast X-Ray Courtesy Ashley Davidoff MD |
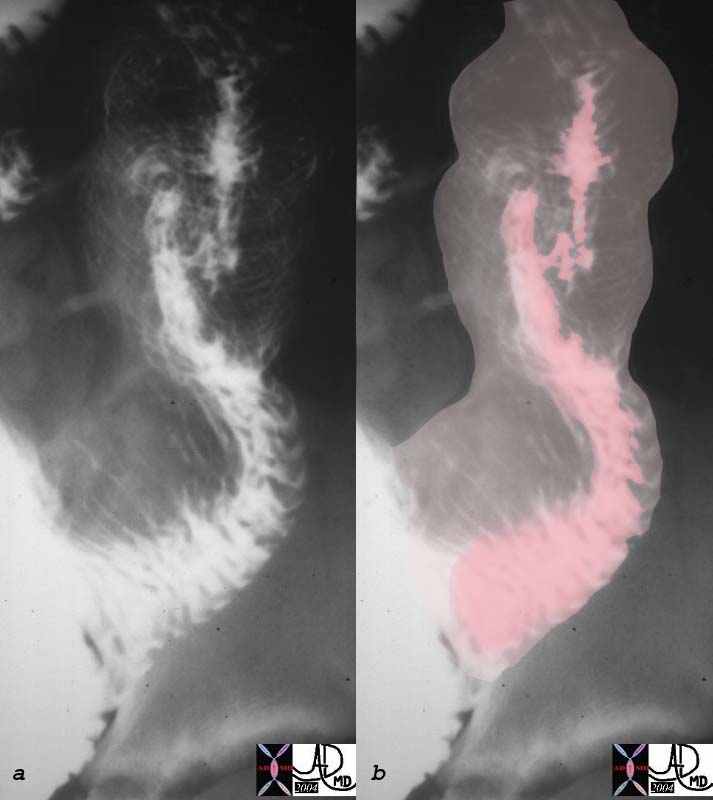 Peutz-Jeghers Syndrome with Intusussception Peutz-Jeghers Syndrome with Intusussception |
| The patient above with polypoid lesions in the small bowel was noted to have intermittant intussusception during the follow through examination. In this image the intussusceptum (pink) is seen within the dilated intussuscipiens where a “stack of coins” or “coil spring effect” of telescoped valvulae are noted.
00512c01 small bowel intussusception upper GI UGI imaging radiology contrast X-Ray fx coil of springs stack of coins dx Peutz- Jeghers Courtesy Ashley Davidoff MD |
Web References
E Medicine Andrea Duchini, MD
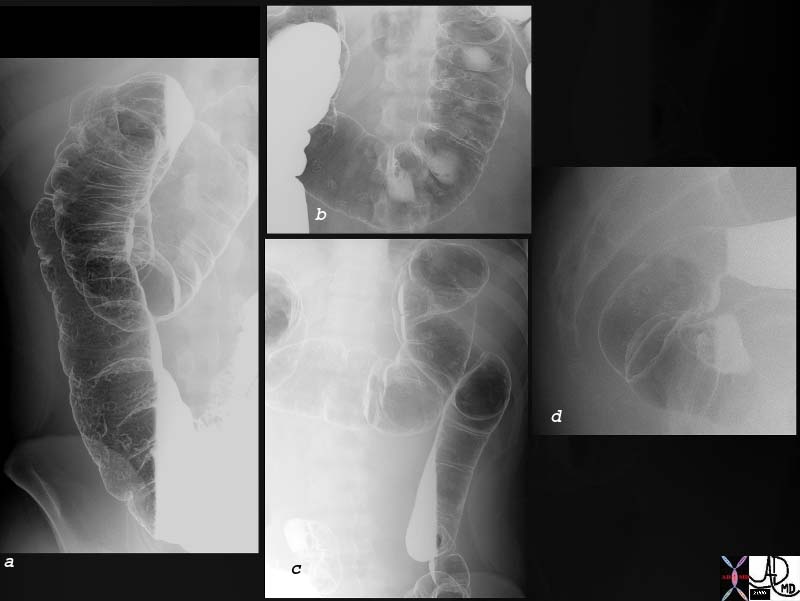 Diffuse Polyposis Diffuse Polyposis |
| 75907c01 young man presents with bloody diarrhea colon ascending colon transverse colon descending colon rectum multiple polyps polyposis double contrast barium enema 75903b01 75901b01 |
Potential Complications
Tubulovillous Adenoma
Clinical
The patients with small polyps are mostly asymptomatic since they do not affect normal function. Bleeding from the polyp may cause hemoccult positivity and if the bleeding is chronic the patient may present with anemia. Some patients with larger polyps may present with intussusception with intermittant colicky abdominal pain.
Diagnosis
Most polyps are adenomatous polyps that develop in the normal colonic mucosa.
Treatment
superficial central ulceration suggestive of malignancy
. In addition to the effect of histologic type on the development of cancer, the size of a polyp is also important. Polyps greater than 2 cm are much more likely to become malignant. Surgery for polyps is indicated in those too larger to remove safely through the colonscope and in those showing carcinoma histologically
Adenocarcinoma of the colon may appear as an ulcerated mass, an annular mass, or as a polypoid, nonulcerated, exophytic mass as shown here. This tumor is obstructing the transverse colon
pseudopolyps is a descriptive term used in pathology and and imaging that relate to islands of normal mucosa surrounded by areas of severe mucosal ulceration often associated with ulcerative colitis
Size Considerations
In general, all polypoid lesions greater than 0.5 cm in diameter identified by colonoscopy, should be totally excised. After removal of a large (>2 cm) sessile polyp repeat colonoscopy should be performed in 3-4 months to evaluate for residual tissue. If present repeat colonoscopic excision should be performed and follow up exam in a further 3-4 months should be performed.
If one benign polyp has been removed then follow up in 3 years is reasonable.
If multiple polyps have previously been excised then follow up is usually recommended in 1 years time
Those that have had carcinoma should be evluated evry 6 months to 1 year
familial adenomatous polyposis (FAP) or Gardner syndrome are recommended to undergo genetic testing and flexible sigmoidoscopy or colonoscopy every 12 months, beginning at age 10-12 years until age 35-40 years if negative. Consider total colectomy for these individuals because they have a nearly 100% risk of developing colon cancer by age 40 years.
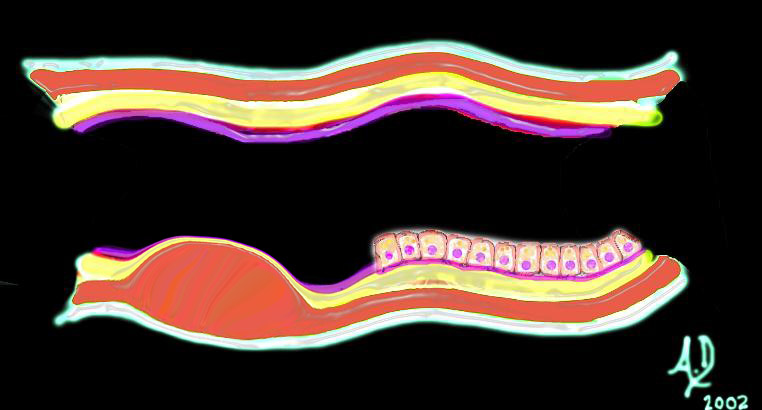
 Malignant and aggressive growth Malignant and aggressive growth |
| The diagram illustrates the transformation from benign to malignant as the neoplasm starts to reveal an aggressive nature and invades and destroys surrounding tissue. In this instance it has advanced into the submucosa and muscularis as well as expanded into the lumen.
Courtesy Ashley Davidoff MD 32362b01 |
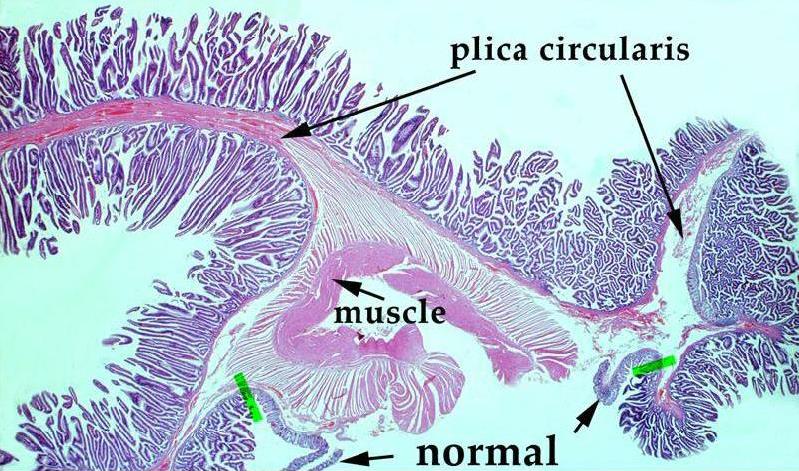
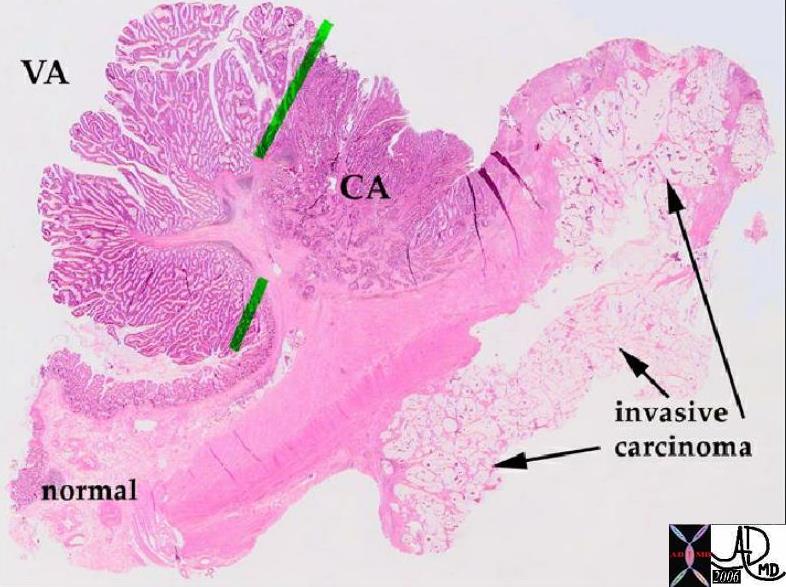 Pathology whole mount showing malignant transformation of a polyp Pathology whole mount showing malignant transformation of a polyp |
| In this pathology specimen the tree like morphology of the polyp is characterized by benign features to the left and superior with malignant features to the right and toward the base rightward and below the green bars. The malignant disease extends into the deeper layers at the base.
Courtesy Barbara Banner MD 12160 |
The finding of a polyp larger than 1 cm in diameter during sigmoidoscopy requires an examination of the rest colon because 30-50% have additional polyps.
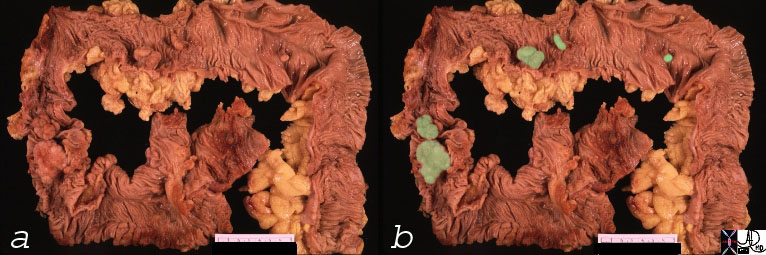 Multiple Polyps Multiple Polyps |
| 00362c01 colon large bowel mass polyp multiple polyps grosspathology Courtesy Barbara Banner MD |
Pseudopolyps
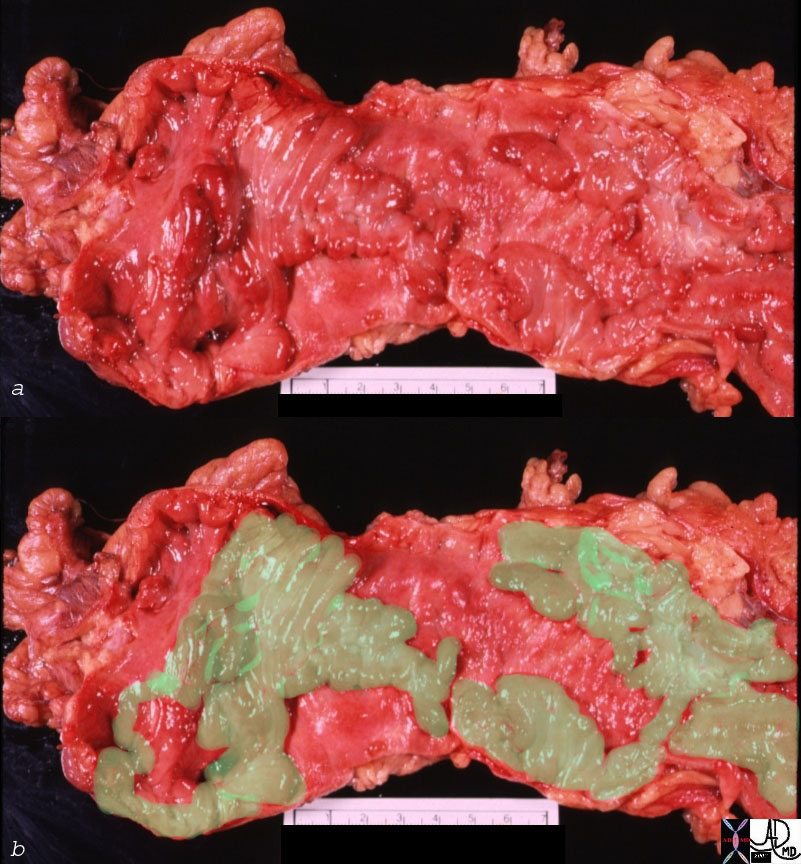 Pseudopolyps Crohn’s Disease Pseudopolyps Crohn’s Disease
Deep Serpigenous Ulcers (red) with Remaining Islands of Normal Tissue (green) |
| 00668c02 colon + fx pseudopolyps fx ulceration dx Crohn’s disease grosspathology aka Crohn’s disease Courtesy Barbara Banner MD Overlay Davidoff MD |
References
Sternbergs Diagnostic Surgical Pathology Volume 2, 4th edition Lippincott Williams Wilkins
Web References
eMedicine Gregory H Enders, MD, PhD, Wafik S El-Deiry, MD, PhD.
Modern Pathology Rhonda K. Yantiss M.D.,Harvey Goldman M.D.and Robert D. Odze M.D., F.R.C.P.C. Hyperplastic Polyp with Epithelial Misplacement (Inverted Hyperplastic Polyp): A Clinicopathologic and Immunohistochemical Study of 19 Cases. Mod Pathol 2001;14(9):869–875
Gastroeneterology Tomonori Yano, Yasushi Sano, Junko Iwasaki, et al. Distribution and prevalence of colorectal hyperplastic polyps using magnifying pan-mucosal chromoendoscopy and its relationship with synchronous colorectal cancer: Prospective study Journal of Gastroenterology and Hepatology Volume 20 Issue 10 Page 1572-1577, October 2005
 12156 colon large bowel fx polyp mass dx villous adenoma benign tumor histopathology mount Courtesy Barbara Banner MD 5star
12156 colon large bowel fx polyp mass dx villous adenoma benign tumor histopathology mount Courtesy Barbara Banner MD 5star