- 24 y/o woman with a question of remote history of a stricture at or near the TI which was thought represnt Crohn’s disease,
- She now presents with
- abdominal pain, fevers, night sweats, diarrhea,
- 25 lbs weight loss
- Subsequently diagnosed
- Tuberculous Enteritis
-

Eye Spy
What do you see?
CT abdomen and pelvis in the coronal plane
Numbered Findings:
1) Enhancing thickened and narrowed terminal ileum (TI) and cecum. 2)Loculated ascites. 3) Omental cake. 4) Free fluid.
Differential Diagnosis:
Malignancy (e.g., Adenocarcinoma or Lymphoma) Gastrointestinal Tuberculosis (GI TB): Crohn’s Disease: Yersinia Enterocolitica Infection: Amoebiasis: Actinomycosis:
Comment: Without clinical context, these findings are nonspecific but suggest pathology in the ileocecal region. Clinical correlation is essential to narrow the differential diagnosis. Each of these entities requires targeted workup and management tailored to the clinical setting.
Credit: Ashley Davidoff MD TheCommonVein.net b1511-01b01ES (02Co)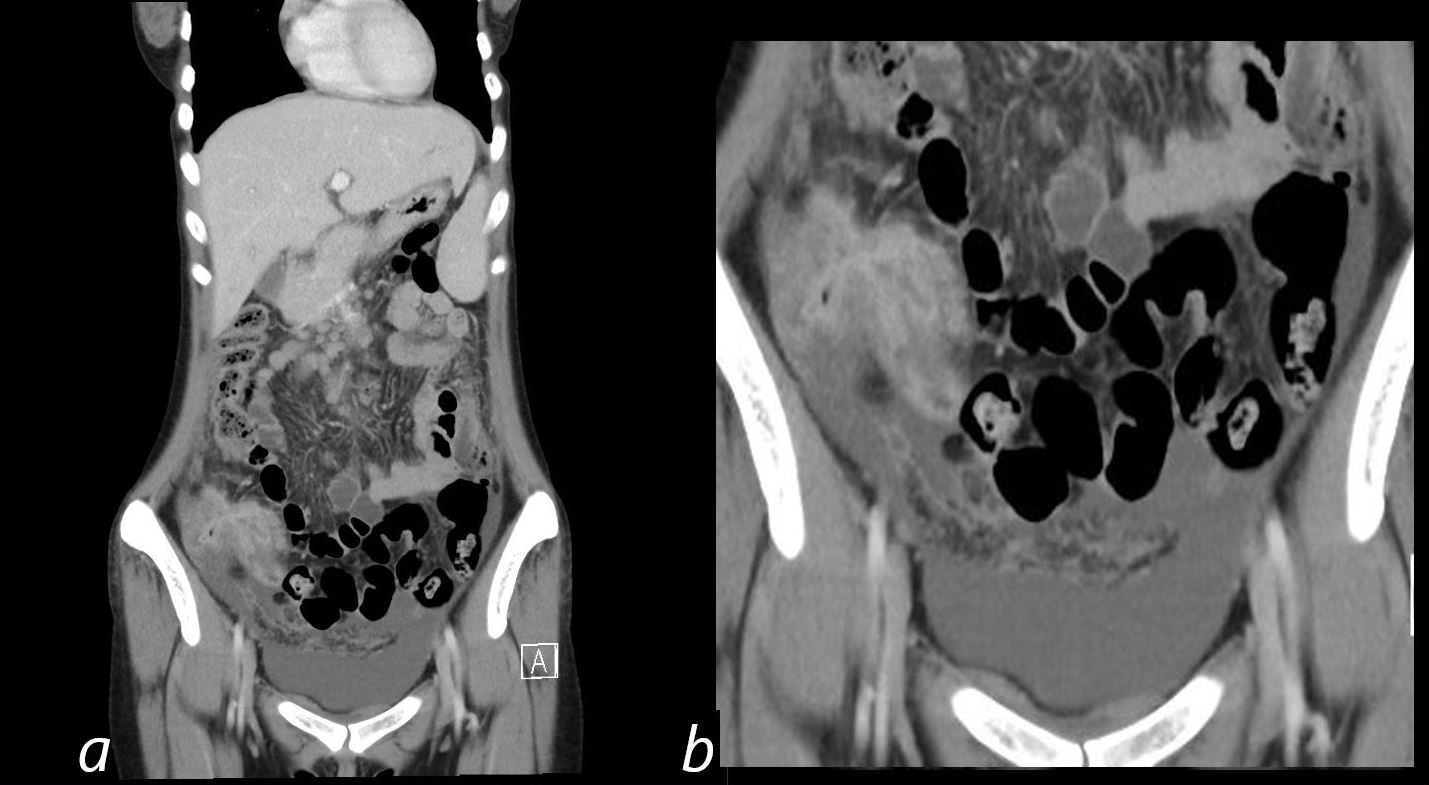
Eye Spy
What do you see?
CT abdomen and pelvis in the coronal plane
Numbered Findings:
1) Enhancing thickened and narrowed terminal ileum (TI) and cecum. 2)Loculated ascites. 3) Omental cake. 4) Free fluid.
Differential Diagnosis:
Malignancy (e.g., Adenocarcinoma or Lymphoma) Gastrointestinal Tuberculosis (GI TB): Crohn’s Disease: Yersinia Enterocolitica Infection: Amoebiasis: Actinomycosis:
Comment: Without clinical context, these findings are nonspecific but suggest pathology in the ileocecal region. Clinical correlation is essential to narrow the differential diagnosis. Each of these entities requires targeted workup and management tailored to the clinical setting.
Credit: Ashley Davidoff MD TheCommonVein.net b1511-00a (02Co)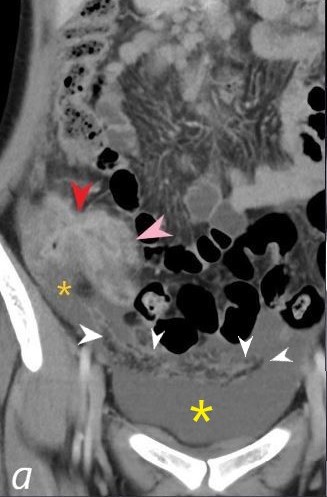
Eye Spy
What do you see?
CT abdomen and pelvis in the coronal plane
Numbered Findings:
1) Enhancing thickened and narrowed terminal ileum (pink arrowhead) and cecum (red arrowhead. 2)Loculated ascites (orange asterisk. 3) Free fluid in the pelvis (yellow asterisk) 4) Omental cake (white arrowheads)
Differential Diagnosis : Malignancy (e.g., Adenocarcinoma or Lymphoma) Gastrointestinal Tuberculosis (GI TB): Crohn’s Disease: Yersinia Enterocolitica Infection: Amoebiasis: Actinomycosis:
Comment: Without clinical context, these findings are nonspecific but suggest pathology in the ileocecal region. Clinical correlation is essential to narrow the differential diagnosis. Each of these entities requires targeted workup and management tailored to the clinical setting.
Credit: Ashley Davidoff MD TheCommonVein.net b1511-01bL01ES (02Co)
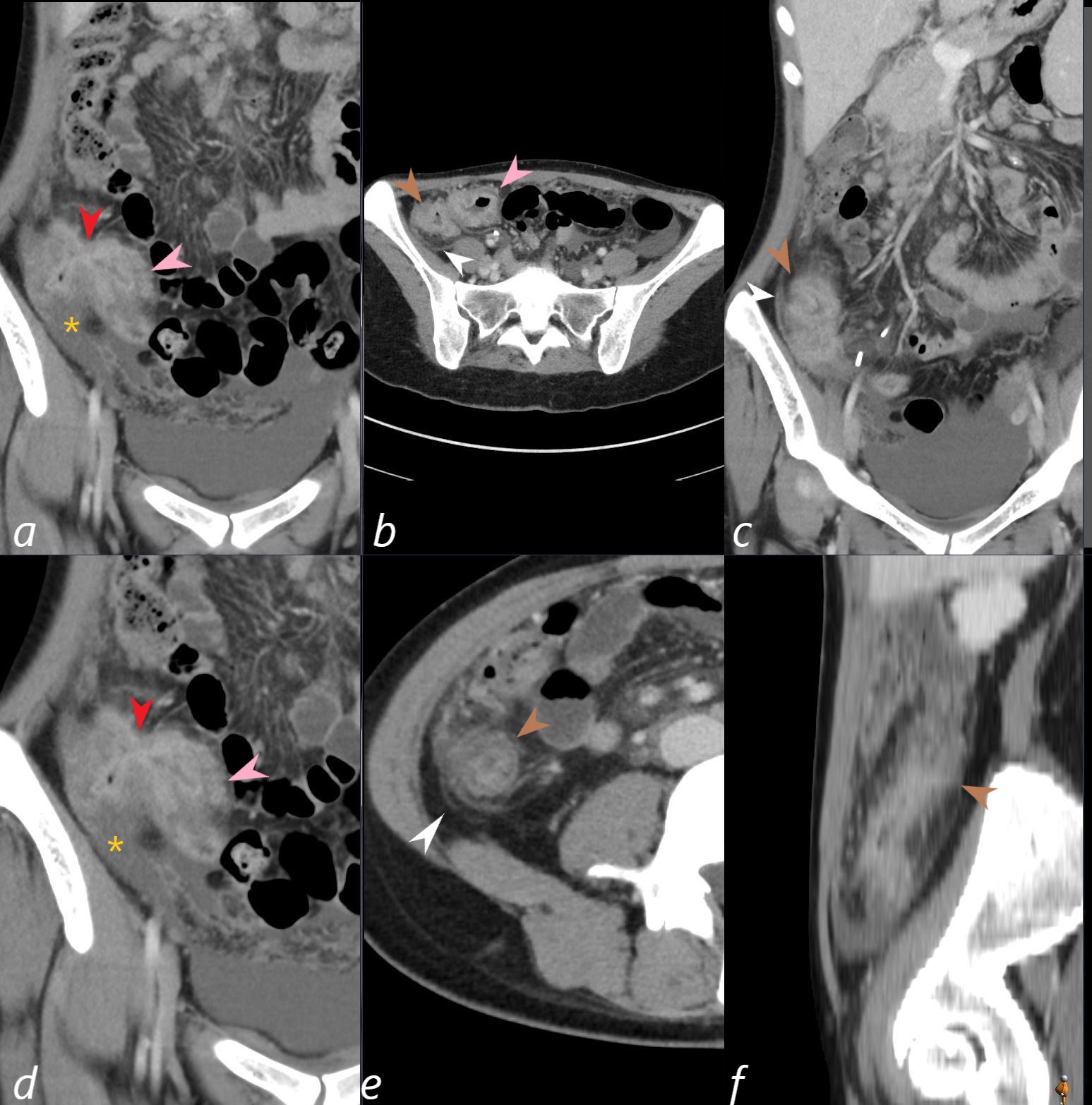
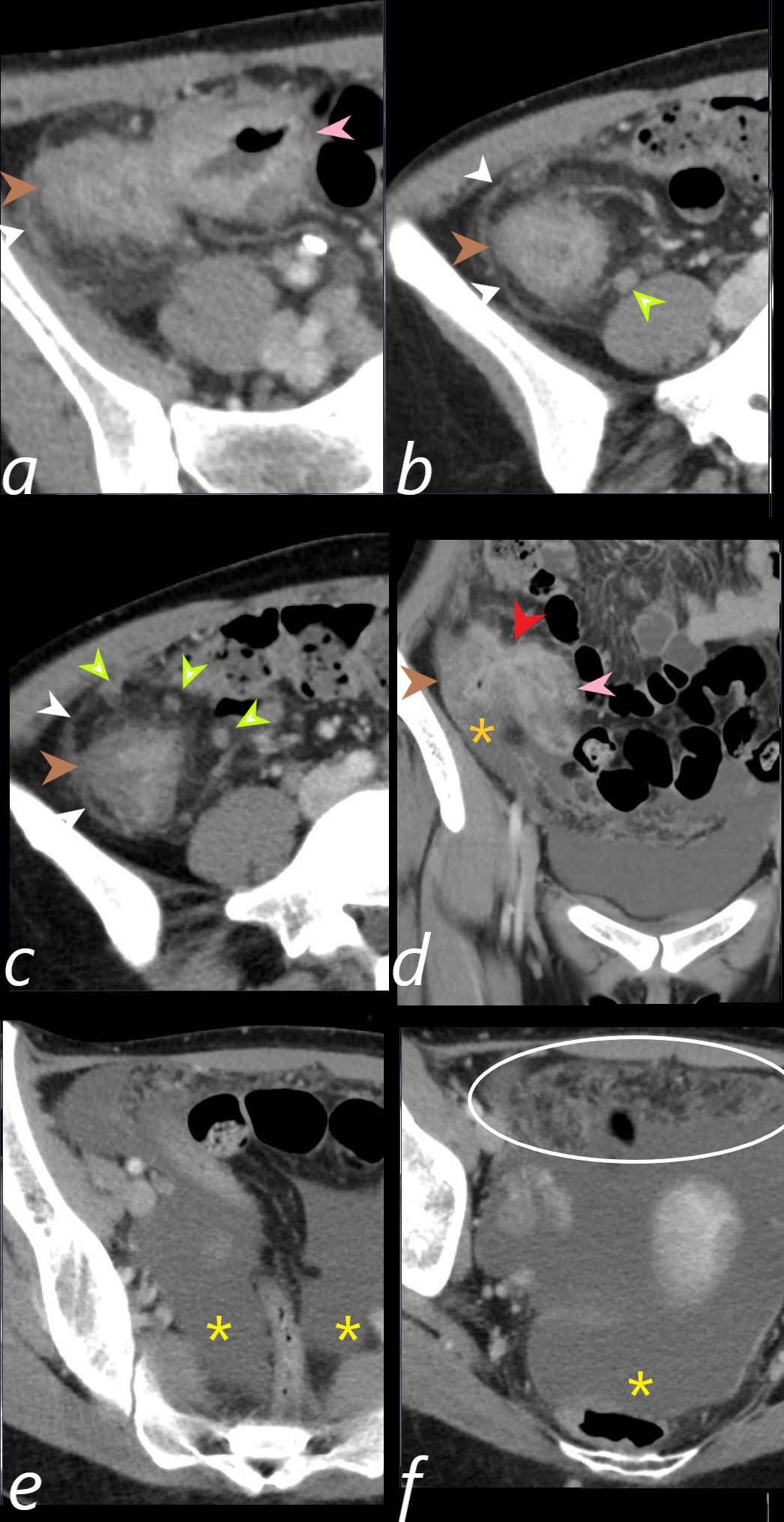
A 24-year-old female presents with abdominal pain, night sweats, and a 25-pound weight loss. CT scan coronal (a, c and d), axial (b and e), and sagittal views (f) show a thickened and enhancing terminal ileum (pink arrowhead a, magnified in d, and also noted in b), a focal stricture (red arrowhead a and d), thickened and enhancing contracted cecum and ascending colon (brown arrowhead b, e, and f) with thickened and indurated pericolic soft tissue and peritoneum (white arrowhead b, c, and e). Loculated ascites is noted alongside the ascending colon (orange asterisk a and d).
Comment:
Findings are consistent with ileo-colitis, and in the appropriate clinical setting, tuberculosis. The differential diagnosis of ileo-colitis includes Crohn’s disease. However, simultaneous continuous involvement of both the ileum and colon without skip areas, as seen in this case, is more characteristic of tuberculosis, while Crohn’s disease typically presents with segmental skip lesions and non-contiguous bowel involvement.
Ashley Davidoff MD TheCommonVein.net b1511-01L (02Co)
Title: Tuberculosis (TB) of the Terminal Ileum and Cecum with Ascites
A 24-year-old female presents with abdominal pain, night sweats, and a 25-pound weight loss.
1511-02L CT axial of the RLQ a,b,c,e,anf f and coronal (d) show evidence of ileo colitis thickening and enhancing ileum (pink arrowhead a, d ) and thickening and enhancing colon (brown arrowhead a, b, c, d) with transmural inflammatory changes ahd peritoneal thickening (white arrowheads a,b, c) . Small enhancing nodes are noted inthe ileocolic region (light green arrowhead b,c) Loculated ascites (orange asteriskd) and free ascites (e,f) Omental induration (omental cake) (white cirle f)
Ashley Davidoff MD TheCommonVein.net b1511-01L (02Co)
Key Features of Tuberculous Peritonitis:
- Caused by hematogenous or lymphatic spread of Mycobacterium tuberculosis or direct spread from an adjacent infected structure (like ileocecal TB).
- Radiologic findings often include:
- Peritoneal thickening and enhancement
- Loculated ascites
- Omental caking due to granulomatous inflammation
- Lymphadenopathy, often with rim enhancement
- Pathophysiology: The infection stimulates a granulomatous reaction with exudative ascites and peritoneal fibrosis.
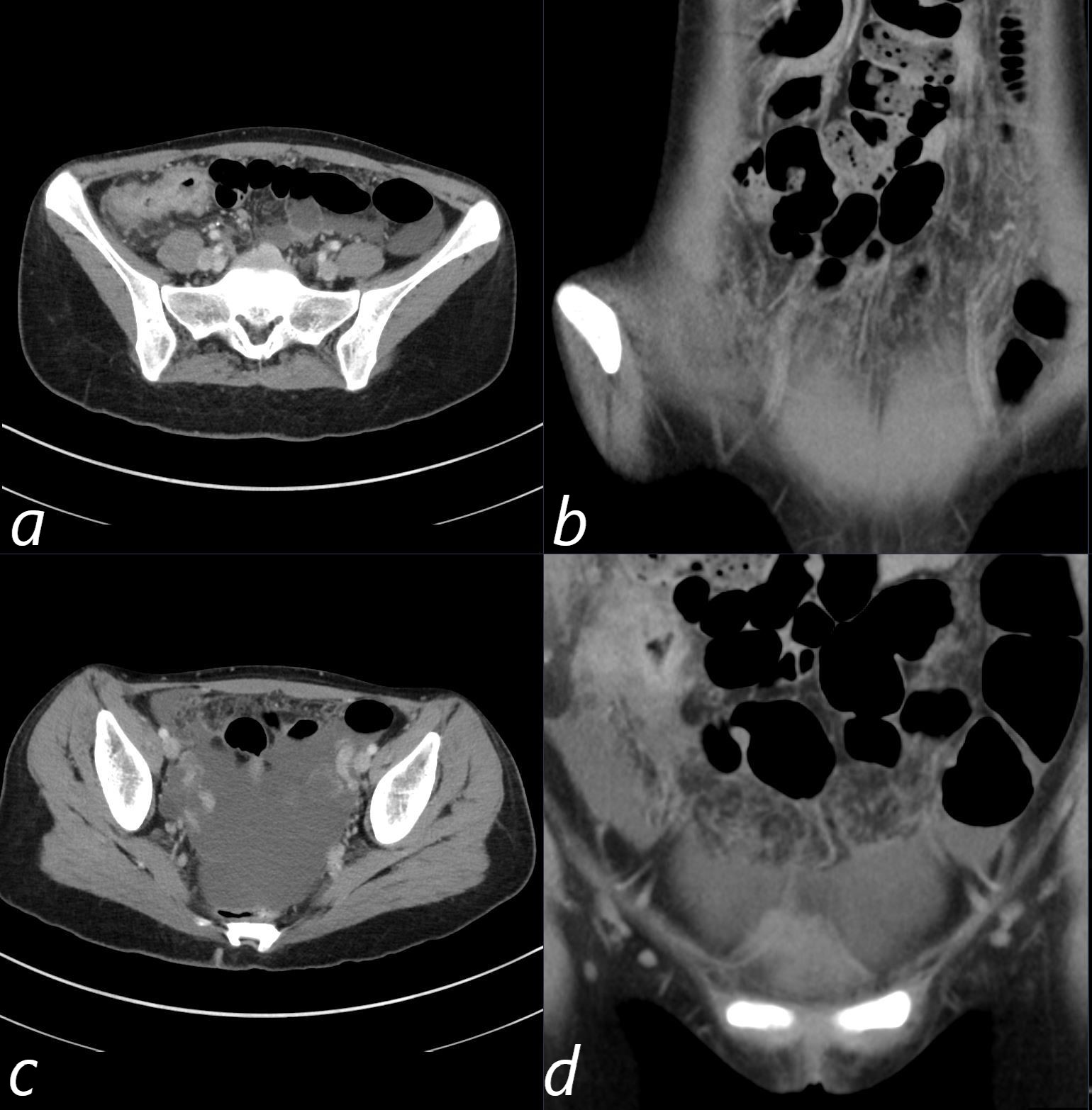
A 24-year-old female presents with abdominal pain, night sweats, and a 25-pound weight loss.
CT axial (a, c) and coronal (b, d) views reveal ileocolic thickening with transmural involvement, induration of the surrounding fat, and thickening of the peritoneum (a). Image (b) shows free ascites and omental caking anteriorly, which is better visualized in the coronal projections (b and d).
Comment: The findings are consistent with tuberculous peritonitis, most likely due to Mycobacterium bovis, which commonly involves the bowel, particularly the ileocecal region, following ingestion of unpasteurized dairy products. The combination of ileocolic thickening, peritoneal enhancement, omental caking, and ascites supports this diagnosis.
Ashley Davidoff MD TheCommonVein.net b1511-03c (02Co)
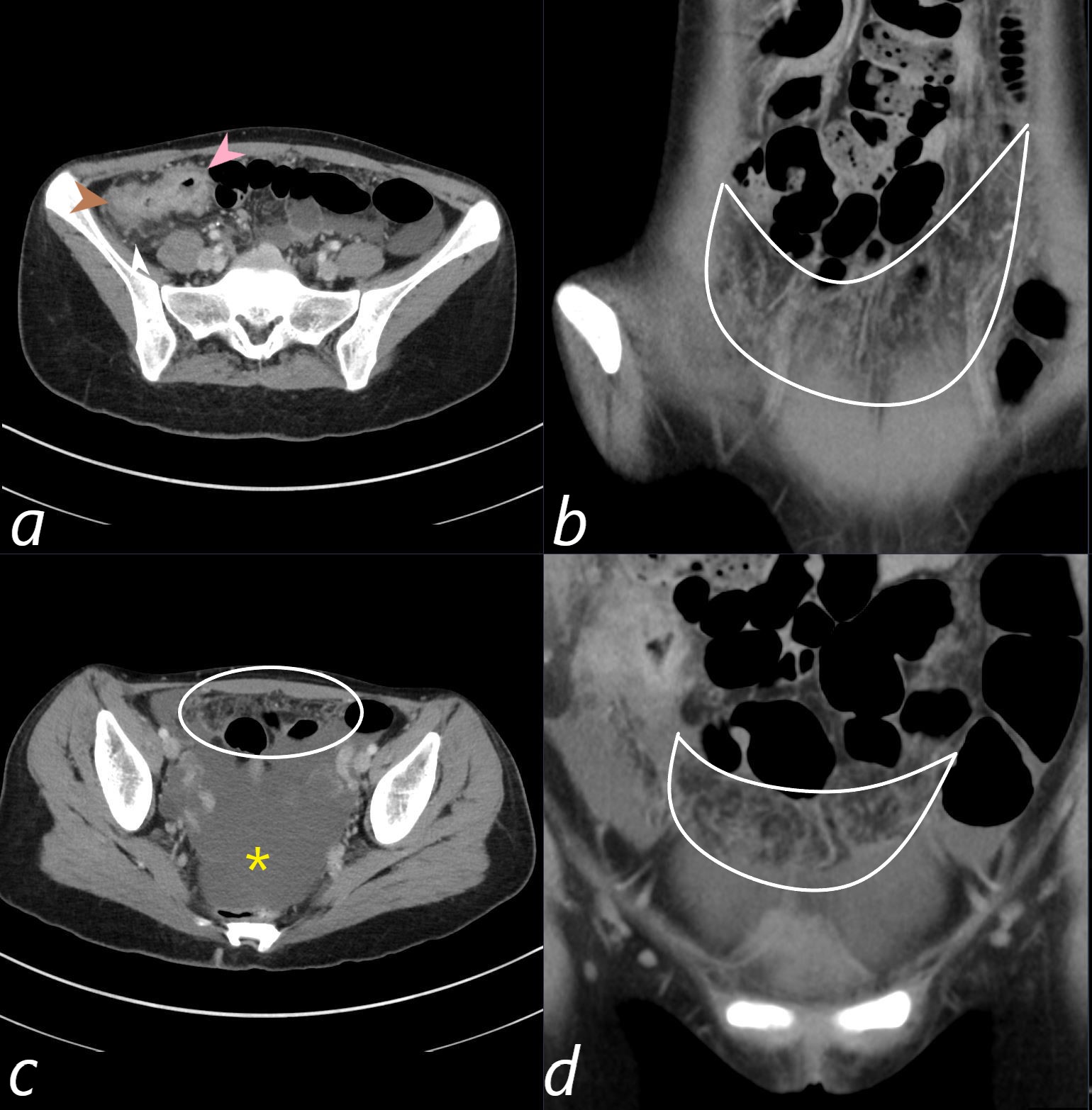
A 24-year-old female presents with abdominal pain, night sweats, and a 25-pound weight loss.
CT axial (a, c) and coronal (b, d) reveal thickening, enhancement, and transmural involvement of the ileum (a, pink arrowhead) and colon (a, brown arrowhead) with induration of the surrounding fat and thickening of the peritoneum (a, white arrowhead). Image (b) shows free ascites (orange asterisk) and omental caking anteriorly (b, white ring). The omental cake is better visualized in the coronal projections (b and d, encircled in white).
Comment: The findings are consistent with tuberculous peritonitis, most likely due to Mycobacterium bovis, which commonly involves the bowel, particularly the ileocecal region, following ingestion of unpasteurized dairy products. The combination of ileocolic thickening, peritoneal enhancement, omental caking, and ascites supports this diagnosis.
Ashley Davidoff MD TheCommonVein.net b1511-03c (02Co)
MRE – MR Enterography
Short segment of wall thickening and enhancement of the terminal ileum and cecal base.
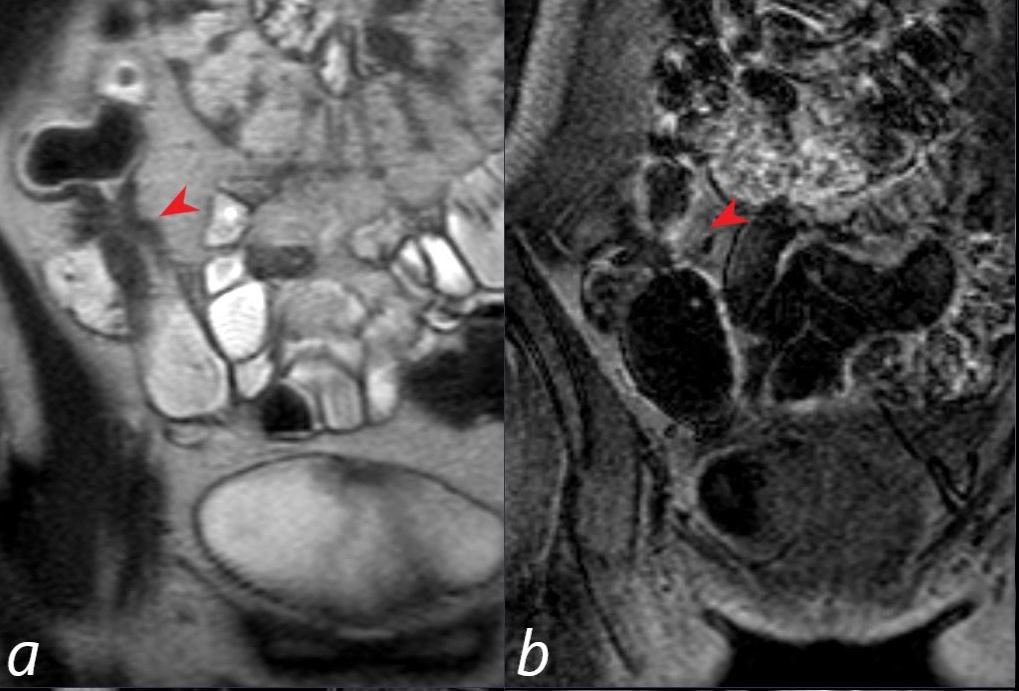
A 24-year-old female presents with abdominal pain, night sweats, and a 25-pound weight loss.
Image a: T2-weighted imaging emphasizing fluid contrast. The red arrowhead indicates a region of narrowing between the terminal ileum (TI) and cecum.
Image b: TFF (Turbo Field Echo), a T1-weighted sequence pre-contrast also shows the region of narrowing (red arrowhead).
Comment: The imaging findings of bowel wall thickening involving the terminal ileum, in this clinical context and in the setting of previous images showing omental caking and complex ascites, are consistent with tuberculous peritonitis.
Ashley Davidoff MD TheCommonVein.net b1511-05bLab (02Co)
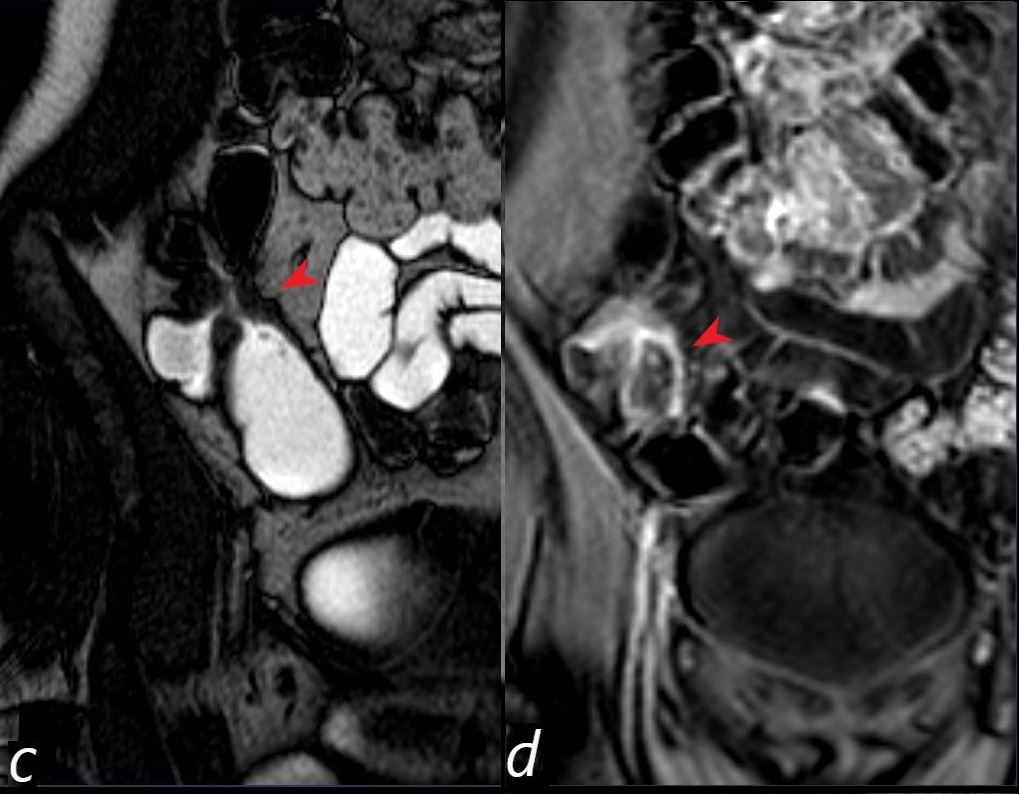
A 24-year-old female presents with abdominal pain, night sweats, and a 25-pound weight loss.
Image a: T2-weighted imaging emphasizing fluid contrast. The red arrowhead indicates a region of narrowing between the terminal ileum (TI) and cecum.
Image c: T2-weighted sequence showing a thin column of fluid in the region of narrowing (red arrowhead).
Image d: THRIVE (T1-weighted) post-contrast imaging with fat suppression, highlighting enhanced bowel wall thickening (red arrowhead)
Comment: The imaging findings of bowel wall thickening involving the terminal ileum, in this clinical context and in the setting of previous images showing omental caking and complex ascites, are consistent with tuberculous peritonitis.
Ashley Davidoff MD TheCommonVein.net b1511-05bLcd (02Co)
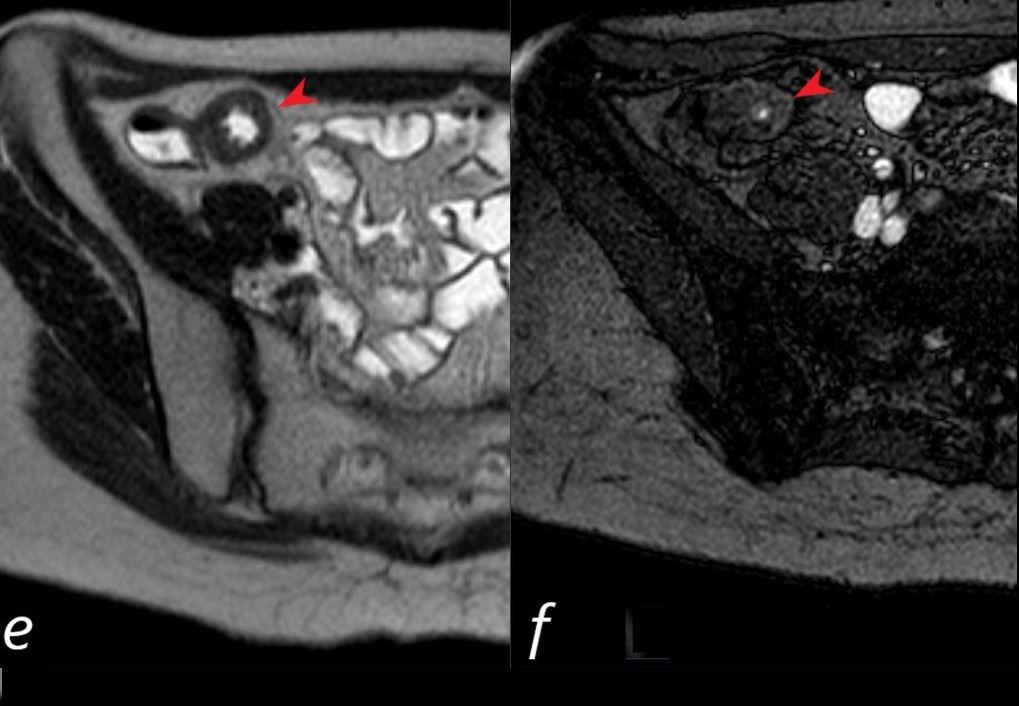
A 24-year-old female presents with abdominal pain, night sweats, and a 25-pound weight loss.
Image e: SS-TSE (T2-weighted) fluid-sensitive imaging showing a thick wall in the region of narrowing surrounding a narrowed lumen with T2-bright fluid (red arrowhead).
Image f: bTFE (Balanced Turbo Field Echo) with both T1 and T2-weighting, where T2 contrast dominates, highlighting the thick wall in the region of narrowing surrounding a very narrowed lumen with T2-bright fluid (red arrowhead).
Comment: The imaging findings of bowel wall thickening involving the terminal ileum, in this clinical context and in the setting of previous images showing omental caking and complex ascites, are consistent with tuberculous peritonitis.
Ashley Davidoff MD TheCommonVein.net b1511-05bL (02Co)
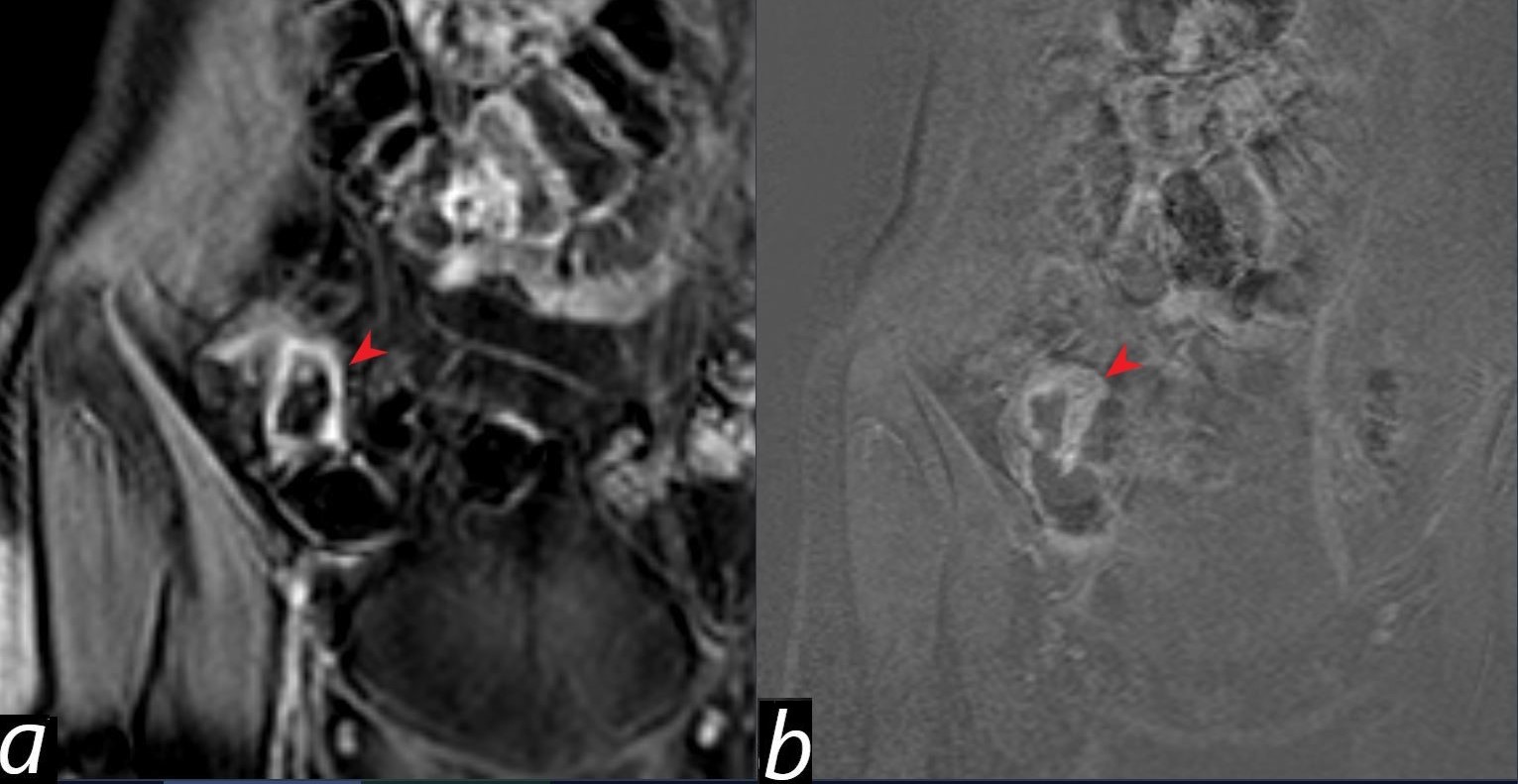
Findings:
Image a: T1-weighted THRIVE post-contrast imaging showing enhancement of the ileocecal region, reflecting active inflammation or hypervascularity (red arrowhead).
Image b: T1-weighted subtraction imaging highlighting enhancement of the thickened ileocecal region, (red arrowhead)., aiding in the differentiation of pathological enhancement from background signal.
Comment:
The ileocecal region is a common site of gastrointestinal tuberculosis due to its rich lymphatic drainage, slow motility, and high absorptive capacity, which predispose it to infection and granulomatous inflammation.
Histology is essential for confirming the diagnosis, typically revealing granulomas with caseous necrosis, characteristic of TB. Acid-fast bacilli (AFB) may also be identified.
The enhancement on post-contrast imaging and subtraction reflects inflammation and hypervascularity, often seen in active TB. These findings emphasize the importance of MRI in assessing bowel wall involvement, vascularity, and associated complications such as ascites or lymphadenopathy.
Credit: Ashley Davidoff MD TheCommonVein.net b1511-051Lgh (02Co)
Colonoscopy:
- Circumferential Ulcers at the cecum with gross deformation of the IC valve. Concern for TB vs. CMV
- Mycobacterum tuberculosis complex as well as positive Quantiferon Gamma Testing.
Pathology:
Treatment with RIPE therapy (6 months)
Follow up
Links and References